Epilepsy & Seizures
Tonic status epilepticus
Jan. 20, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Epilepsy with eyelid myoclonia with absences is a form of epileptic seizure manifesting with myoclonic jerks of the eyelids, often with brief absences. Epilepsy with eyelid myoclonia and absences (formerly Jeavons syndrome) is characterized by unique clinical and EEG features, which follow eye closure in the light and are pathognomonic of this syndrome. Slow eye closure (voluntary or on command) in the light induces eyelid myoclonia, upward deviation of the eyeballs and head, in association with generalized polyspike-wave or spike-wave EEG discharges 3 to 6 Hz. The concomitant absence may be conspicuous or inconspicuous relevant to the duration of brief generalized discharge. These discharges and clinical phenomena are invariably evoked during intermittent photic stimulation, not only on eye closure but also with the eyes opened. The electroclinical phenomena that follow eye-closure disappear when the eyes open and remain opened. Most authors support the view that eyelid myoclonia on eye closure is the defining seizure type of a generalized epilepsy syndrome, which is genetically determined, has age-related onset, and affects otherwise normal children, with a female preponderance. Epilepsy with eyelid myoclonia with absences is probably lifelong, with continuing seizures in adult life. Eyelid myoclonia is often confused with facial tics or self-induction of seizures. In this article, the author details developments in the clinical manifestations, pathophysiology, genetics, and pharmacological treatment of eyelid myoclonia with absences.
|
• Eyelid myoclonia with absences is a distinct type of epileptic seizure that is often misdiagnosed as facial tics or another nonepileptic paroxysmal event of eyelid jerking. | |
|
• The characteristic eyelid myoclonia on eye closure, if seen once, will never be forgotten or confused with other conditions. | |
|
• A main misconception is that eyelid myoclonia with or without absences is an attempt to self-induce seizures. | |
|
• Epilepsy with eyelid myoclonia with absences is a genetic generalized epilepsy syndrome characterized by eyelid myoclonia and absences on voluntary or on command eye closure in the light. Eye closure in the dark or passive eye closure does not trigger clinical symptoms or EEG discharges. | |
|
• Myoclonic and absence seizures are the predominant seizure types in the syndrome epilepsy with eyelid myoclonia, previously known as Jeavons syndrome. |
The first documentation of eyelid myoclonia was by Radovici and colleagues (93).
In 1977, Jeavons described “eyelid myoclonia and absences” as follows: “There is marked jerking of the eyelids associated with 3 c/s SWDs or Poly-SWDs often irregular, immediately after eye closure and invariably positive response to intermittent photic stimulation (IPS). The mean age of onset is 6 years and female predominate...” (53):
|
Therefore, eyelid myoclonia and absences show a marked jerking of the eyelids immediately after eye-closure and there is an associated brief bilateral spike and wave activity. The eyelid movement is like rapid blinking and the eyes deviate upwards, in contrast to the very slight flicker of eyelids which may be seen in a typical absence in which the eyes look straight ahead. Brief absences may occur spontaneously and are accompanied by 3 Hz spike and wave discharges... The spike-and-wave discharge seen immediately after eye closure does not occur in the dark. Generalized spike-wave discharges evoked immediately after eye closure during the baseline EEG are a very reliable warning that abnormality will be evoked by photic stimulation. The mean age of onset is 6 years. |
Eyelid myoclonia with absences has been studied extensively (32; 50; 05; 09; 40; 48; 85; 87; 106; 104; 39; 83; 84; 23; 25; 26; 55; 18; 19; 91; 114; 76). However, eyelid myoclonia with or without absences, induced by eye closure and photic stimulation (previously known as Jeavons syndrome) has been recognized as a distinct genetic generalized epilepsy syndrome by the International League Against Epilepsy (101). The mandatory seizures are brief, repetitive, often rhythmic, fast (4 to 6 Hz) myoclonic jerks of the eyelids with simultaneous upward deviations of the eyeballs and extension of the head. All patients are photosensitive, and eyelid myoclonic status epilepticus may occur in up to one fifth of patients (101).
Although the triad of epilepsy with eyelid myoclonia is well defined with eyelid myoclonia, eye closure-induced EEG paroxysms and seizures, and photosensitivity, the syndrome has been recognized since 1977. However, many cases are underdiagnosed or misdiagnosed (53). In a comprehensive narrative review, there was a strong consensus among panelists that eyelid myoclonia may be present for many years prior to recognition as a seizure and that eyelid myoclonia may be inappropriately diagnosed as ocular tics (99).
This article and other publications present a significant number of video-EEG recordings documenting the fact that eyelid myoclonia is the more obvious clinical manifestation and can also occur alone without impairment of consciousness (15; 83; 23; 52; 14).
Eyelid myoclonia and absences have two components. The initial and more prominent of these components is eyelid myoclonia, and the second component is the concomitant conspicuous or inconspicuous absence seizure. These unique clinical features that occur immediately after voluntary or on command eye closure in the light are associated with generalized spike-and-wave discharges and are characteristic of the syndrome eyelid myoclonia with absences. The electroclinical phenomena vanish on eye opening and are enhanced during drowsiness, hyperventilation, and intermittent photic stimulation. During photic stimulation, myoclonic jerks other than eyelid myoclonia are commonly evoked on eye closure and may precede or follow a brief absence. Absence and myoclonic jerks can also be provoked with the eyes open in some classical cases.
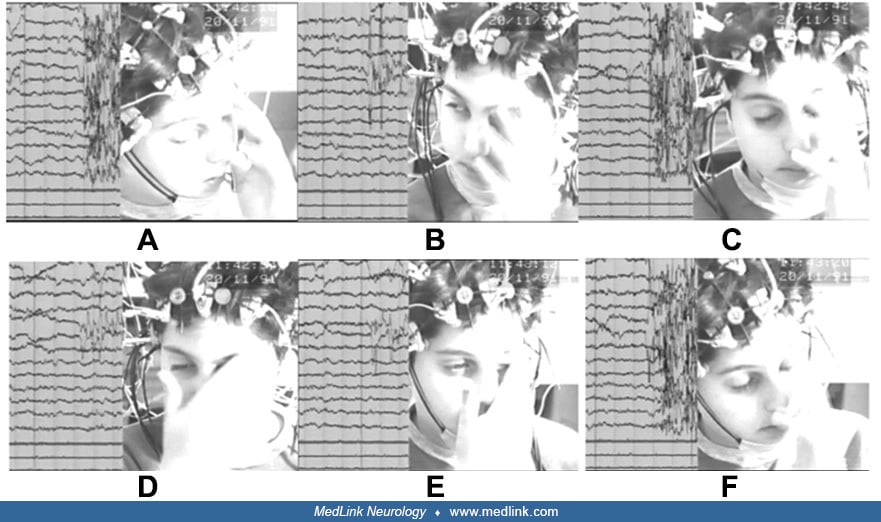
Eyelid myoclonia with absences is an idiopathic/genetic generalized epilepsy in which myoclonic seizures (eyelid myoclonia and myoclonic jerks other than eyelid), absence seizures, and generalized tonic-clonic seizures contribute to the clinical phenotype to a variable degree (25). In a few cases, a tonic eyelid spasm is recorded on EEG at the end of eye closure as a plateau before the eyelids open and jerk in concordance with a jerk of the upper part of the body and generalized spike-wave discharges.
Video-EEG of a 7-year-old girl with a 6-month history of eyelid jerks and occasional myoclonic jerks in the light. When instructed to close her eyes, her eyes slowly closed. After a brief period of palpebral tonic spasm (platea...
Since 1977, when Jeavons described eyelid myoclonia and absences as a separate type of photosensitive epilepsy, many publications refer to eyelid myoclonia with absences or without absences. However, the term “eyelid myoclonia and absences,” as initially reported, better expresses the characteristic phenotype of Jeavons syndrome because absence seizures may occur independently of eye closure during hyperventilation and intermittent photic stimulation (24; 25; 26). Myoclonic seizures other than eyelid are reported in 34% to 54.5% of cases (48; 24; 25). Generalized tonic-clonic seizures are seen in 50% of cases and are the usual presenting symptom in mild forms (24; 25). In a publication of 40 cases with eyelid myoclonia with absences, eyelid myoclonias were present at the onset in 29 patients (72.5%), and generalized tonic-clonic seizures were present in 11 (27.5%) (77). However, over the course of the disease, all had absences.
Eyelid myoclonia. Eyelid myoclonia on eye closure, voluntary or on command, in light of variable intensity represents the hallmark of eyelid myoclonia with absences (previously known as Jeavons syndrome). An eyelid flutter may be associated with generalized beta, theta, or delta rhythm on EEG as well as a marked eyelid jerking concomitant with an upward deviation of the eyeballs and retropulsive head movement, with generalized polyspike-and-wave or spike-and-wave discharges ranging from 3 to 6 Hz that are often irregular and fragmented.
In some cases, if the eyelid jerking is marked, the person is unable to control their eyes when open; they close again following the person’s urge to close their eyes according to the command ‘‘close your eyes’’ given by the technician. As a result, similar clinical phenomena are reproduced. This repetition of events may continue for a few seconds, and the concomitant EEG discharges appear irregular and fragmented. After a few repeats of clinical and EEG phenomena, the patient manages to control their eyes when open and returns to the normal baseline state with a sigh of relief (25). The eyelid movements are rhythmic, repetitive, slight or marked, and single or multiple, even in the same patient. Phenotypic variability exists not only among individuals, but also within the same individual—a projection of genetic variation and brain maturity level.
Absence seizures. Conspicuous or inconspicuous absence seizures, concomitant with eyelid myoclonia on eye closure, are almost always present and usually very brief, requiring a very meticulous video-EEG assessment. The longer the concomitant generalized spike-wave discharges are, the more obvious the absence. Absence seizures can also be observed during hyperventilation and intermittent photic stimulation, with the eyes opened.
Myoclonic seizures. Myoclonic seizures other than eyelid have been reported to occur in children (34%) (25) and in adults (54.5%) (48). The majority of cases occur either independently or in association with eyelid jerking on eye closure (53; 24; 25; 83). The jerks, subjective or objective, usually involve the upper part of the body. The head may jerk to one side or be drawn to one side like a magnet (nodding, shaking). Myoclonic jerks during voluntary or on command eye closure may be preceded or followed by a brief absence and are commonly induced during photic stimulation (24; 25).
Generalized tonic-clonic seizures. Generalized tonic-clonic seizures are the usual referral symptom in mild or classical types of eyelid myoclonia and absences and occur in about 50% of cases, particularly those receiving no treatment or treated unsuccessfully or inappropriately. Generalized tonic-clonic seizures are usually precipitated by drowsiness, sleep deprivation, fatigue, bright or flashing lights, and alcohol abuse associated with sleep deprivation. In cases that show marked photosensitivity, perpetuating the photic stimulation may lead to a generalized tonic-clonic seizure. An indication that heralds such an event is repetition of generalized spike-and-wave discharges during the same flash frequency.
Nonconvulsive status epilepticus in eyelid myoclonia and absences. Exceptionally, eyelid myoclonia with absences may present as nonconvulsive status epilepticus. The main presenting symptoms are prolonged confusion states. Routine electroclinical assessment reveals the typical characteristics of seizures associated with eyelid myoclonia and absences on eye closure. Photosensitivity is usually marked and may lead to a generalized tonic-clonic seizure (26).
The relationship between eyelid myoclonia with absences and epileptic negative myoclonus has not previously been reported. In one publication, it was reported in a 10-year-old girl who presented with eyelid myoclonia, eye closure-induced paroxysms, and photosensitivity; an ictal EEG depicted an eye closure-induced diffuse 3.0 to 4.5 Hz polyspike-and-wave complex, which was accompanied by eyelid myoclonia (31). The electromyography disclosed a brief interruption (60 to 140 msec) of tonic contraction of the orbicularis oculi muscle, which was associated with the polyspike-and-wave complex on EEG. The findings led to the diagnosis of epileptic negative myoclonus. They concluded that eye closure–induced eyelid epileptic negative myoclonus may be an atypical seizure type of eyelid myoclonia with absences that represents an intermediate between eyelid myoclonia and epileptic negative myoclonus (31).
Eyelid myoclonia and absences has been described as a photosensitive epilepsy syndrome since 1977 (53); it has been underdiagnosed and or misdiagnosed. The syndrome is characterized by unique clinical and EEG features, which follow eye closure (voluntary or on command) and are pathognomonic of this syndrome. Eye closure in the light induces eyelid flicker, flutter, or jerking in association with EEG paroxysms and seizures. All patients are photosensitive. Absence seizure and generalized tonic-clonic seizures do occur. The clinical and EEG paroxysms are not triggered in the dark and on passive eye closure (24; 25; 26). It is classified as early onset (typical, atypical), mild form, classical type, and epilepsy with eyelid myoclonia combined with juvenile myoclonic epilepsy (26). Myoclonic seizures, other than eyelid, in adults and in children have been reported to occur in 54.5% and 34%, respectively (48; 25; 26), and generalized tonic-clonic seizures occurred in about 50% of the reported cases and were usually the referral symptom in the mild or the classical form of either untreated or treated unsuccessfully or with inappropriate antiseizure medication (24; 26).
Early-onset eyelid myoclonia and absences (under 4 years of age).
Typical form. The characteristic electroclinical phenomena of eyelid myoclonia with absences, previously known as Jeavons syndrome, are easily diagnosed and differentiated from other idiopathic generalized epilepsies appearing early in life. For example, juvenile myoclonic epilepsy (JME), which is officially recognized as a syndrome, may appear in children under the age of 4 years with myoclonic seizures with or without absences, but the diagnosis of juvenile myoclonic epilepsy syndrome is made in childhood after treatment is discontinued and relapses occur. In eyelid myoclonia and absences, the frequent and brief (1 to 3 seconds) absence seizures with upward deviation of the eyes, which are triggered by eye closure in the light or photic stimuli, are characteristic and not seen in typical absence seizures of early onset. EEG demonstrates 3- to 5-Hz spike-and-slow-wave activity on eye closure and intermittent photic stimulation but also spontaneously.
An Xq25 microduplication involving the whole STAG2 gene was reported in an 8-year-old boy with eyelid myoclonia and absences, mild intellectual disability, speech delay, and onset at 3 years of age, fulfilling all electroclinical criteria of what was formally named Jeavons syndrome (51). Array CGH identified that a 199 kb copy number gain in Xq25, including the whole STAG2 gene, was inherited from his asymptomatic mother.
In one study by Spurgeon and colleagues, a heterozygous mutation in the PLCB1 gene, which has been linked to early onset epilepsies and encephalopathic epilepsies, was reported in a 7-year-old female who presented with eyelid myoclonia, which was evident since birth with absence seizures and migraines with associated photosensitivity, but was diagnosed as Jeavons syndrome (102).
It seems that early-onset eyelid myoclonia with absence seizures triggered by eye closure (eye closure sensitivity) is associated with a poorer response to antiseizure medication, a higher rate of cognitive dysfunction, and psychiatric comorbidities relevant to the underlying genetic expression.
Atypical form. The presentation of the atypical form is with frequent generalized tonic-clonic seizures in the first year of life. Sodium-channel blockers provoke absence and myoclonic seizures and eyelid jerking; other myoclonic jerks usually become apparent during infancy. EEG shows frequent brief and irregular generalized 2- to 3-Hz spike-waves and polyspike and slow-wave discharges, particularly on eye closure with concomitant eyelid jerking and occasional jerks of the upper limbs. Photosensitivity is usually marked. Focal spike or spike-and-slow-wave complexes are also seen. MRI is normal. The children show moderate intellectual disability.
Mild form eyelid myoclonia and absences. It may be months or years before a person with eyelid fluttering after eye closure seeks medical advice for an occasional generalized tonic-clonic seizure. EEG shows abnormalities on eye closure and positive response to intermittent photic stimulation. Some milder cases with 1, or even 2, generalized tonic-clonic seizures in their lifetime never seek treatment.
Case presentation. The patient presented at the age of 12.5 years, after a generalized tonic-clonic seizure provoked by drowsiness. She recalled having rare myoclonic jerks since the age of 12, particularly during the summer, when she was looking at the sun’s reflection on seawater. She also remembered some unilateral jerks involving the upper limbs. Her sleep-awake video-EEG showed polyspike-wave complexes in the frontal regions and single or up to 3-second-long generalized spike-and-wave discharges, which were maximal over the frontal regions during sleep. Hyperventilation increased the generalized 3- to 5-Hz spike-and-wave discharges of 1- to 3-second duration, which were almost always after eye closure and associated with eyelid flutter and some jerks of the head or arms. The photosensitivity range on eye closure was 1 to 60 Hz; with the eyes open, it was 7 to 30 Hz. Most of the discharges were typical, with concomitant eyelid flutter and spontaneous eye opening and staring. Some frequencies evoked myoclonic jerks. She was put on levetiracetam.
Her mother, aged 33, was noticed to have eyelid flutter on eye closure. On direct questioning, she remembered that her father and his sister also had eyelid fluttering or jerking on eye closure. On waking, the mother’s EEG showed brief discharges of fast activity or irregular generalized spike-and-wave discharges on eye closure with eyelid flutter during the hyperventilation. She had never asked for medical advice and had never had any generalized tonic-clonic seizures.
Classical eyelid myoclonia and absences. In classical eyelid myoclonia and absences, there is marked jerking of the eyelids, often with upward deviation of the eyes and retropulsive movements of the head, immediately after eye closure that are associated with generalized spike-wave discharges on EEG. In all cases, eyelid myoclonia is associated with absences, and the positive response to intermittent photic stimulation and pattern is usually marked.
When asked about their feelings during the events, people with eyelid myoclonia and absences are often unable to explain the feeling, but admit it is rather relieving or pleasant.
Eyelid myoclonia with absences and juvenile myoclonic epilepsy. In some cases, the presenting symptom is myoclonic jerks of the arms on awakening, suggesting juvenile myoclonic epilepsy. During the sleep-awake video-polygraphic EEG following sleep deprivation, typical eyelid myoclonia associated with myoclonic jerks and generalized spike-wave discharges are observed on eye closure. All cases are photosensitive, and hyperventilation and intermittent photic stimulation provoke clinical and generalized EEG discharges. Generalized tonic-clonic seizures may occur.
Rarely, epilepsy with eyelid myoclonia presents with nonconvulsive status epilepticus. The main presenting symptoms are prolonged confusion states of varying severity. Photosensitivity is usually marked and may lead to a generalized tonic-clonic seizure (25; 26).
Headache and eyelid myoclonia. Ictal headache has been associated with eyelid myoclonia in only one report (38).
Precipitating factors of eyelid myoclonia and absences. The most potent precipitating factor is eye closure, voluntary or on command, in the light. Other precipitating factors are sleep deprivation, bright light or flashing lights, drowsiness, fatigue, alcohol abuse associated with sleep deprivation, and drug-resistant or inappropriate treatment or noncompliance (24). Photosensitivity declines with age, whereas eye closure is likely to remain a lifelong precipitating factor (48) or even continue, in some cases, as a habit after the self-limitation of the epileptic events in adulthood (24; 25).
In a study of 80 cases with epilepsy with eyelid myoclonia, it was reported that eye closure sensitivity was more common than photosensitivity (78). Photosensitivity was more likely to disappear than eye closure sensitivity, and both eye closure and intermittent photic stimulation could induce three grades of interictal and ictal epileptiform discharges (I, focal posterior; II, the posterior spread into the frontal; and III, generalized), confirming that visual stimuli could trigger occipital cortex originating epileptic neural network to varying degrees. This further recognizes epilepsy with eyelid myoclonia as another continuum epilepsy.
In another multicenter retrospective cohort study, 267 patients with epilepsy with eyelid myoclonia from nine countries were included (20). They classified three subgroups: early onset, intermediate onset, and late onset. The early-onset epilepsy with eyelid myoclonia subgroup was associated with the highest rate of intellectual disability, antiseizure medication refractoriness, and psychiatric comorbidities and with the lowest rate of family history of epilepsy. The late-onset subgroup was associated with the highest proportion of body myoclonia and generalized tonic–clonic seizures, whereas the intermediate-onset epilepsy with eyelid myoclonia subgroup had the lowest observed rate of additional findings. A family history of epilepsy with eyelid myoclonia was significantly more frequent in intermediate- and late-onset epilepsy with eyelid myoclonia compared with early-onset epilepsy with eyelid myoclonia (20).
Eyelid myoclonia is highly resistant to treatment, occurring many times per day, often without apparent absences, and even without demonstrable photosensitivity. Generalized tonic-clonic seizures and absence status may be unavoidable in adult life, either as the result of accumulating precipitating factors, or more often, due to inappropriate medication (83; 84). Neuropsychological evaluations of patients showed that performance was below average on measures of global IQ, processing speed and rote, verbal learning coupled with average nonverbal reasoning, and sustained attention (45). There was also evidence of impaired higher-level verbal reasoning. Although global IQ ranged from low average to borderline impaired, no participant could be accurately described as impaired or having intellectual disability given the consistently average performance noted on some higher-order tasks, including nonverbal reasoning. A patient with eyelid myoclonia with absences showed significantly higher impulsivity compared to healthy controls and those with juvenile myoclonic epilepsy, and impulsivity was higher in those treated with levetiracetam (67).
Eyelid myoclonia with absences is a generalized epileptic seizure with generalized multiple spike-and-slow-wave discharges that may be of higher amplitude in the anterior or posterior regions.
Eyelid myoclonia (the seizure) may occur in various conditions. Eyelid myoclonia with absences is a genetically determined condition that may be different from most other idiopathic generalized epilepsy syndromes. Bianchi and colleagues reported that the familial preponderance and concordance in families of probands with eyelid myoclonia with absences is high (09). Parker and colleagues reported that of 18 patients with eyelid myoclonia with absences, 14 had a family history of epilepsies (90). Four patients had other family members affected by a similar type of epileptic condition. Eyelid myoclonia with absences in monozygotic twins has been reported (01). Rarely, benign myoclonic epilepsy of infancy (75) or cryptogenic myoclonic epilepsy of early childhood (79) may evolve into eyelid myoclonia with absences. In a 2005 study based on 50 cases, it was reported that the family history of eyelid myoclonia and absences induced by eye closure in the light was 28%, and among them, there were nine families of probands with eyelid myoclonia with absences and first-degree relatives with eyelid myoclonia and absences or idiopathic generalized epilepsy (24). The concordance rate was 78%, indicating a dominant mode of inheritance. In another study, the family history for epilepsy was 39.5%, the majority with idiopathic generalized epilepsy, and the family history for febrile seizures was 9.5% (19). Familial cases have been reported in other studies (34; 01; 96) and in monozygotic male twins of Chinese origin, associated with absence status (126). In another report, six of 108 children with childhood absence epilepsy later developed eyelid myoclonia with absences after treatment withdrawal (47).
Rudolf and colleagues performed whole-exome sequencing in a family with eyelid myoclonia with absences (94). They identified an inherited nonsense variant in the RORB (retinoid-related nuclear receptor) gene, which encodes the retinoid-related nuclear receptor ROR-beta, as a new candidate gene for neurodevelopmental disorders, including epilepsy and especially in generalized epilepsies with predominant absence seizures. A de novo mutation of the RORB gene was described in a patient with eyelid myoclonia with absences, intellectual disability, and attention deficit hyperactivity disorder (74). The RORB gene is involved in vivo in different neuronal processes, among which are migration and differentiation. The phenotype associated with RORB variants has also been expanded, making it the first gene to be associated with the overlap of photosensitive genetic generalized and occipital epilepsy (95). A KCNB1 mutation was reported in six patients with early-onset generalized and focal epilepsies, including a case diagnosed as eyelid myoclonia with absences (68). Furthermore, evidence has suggested mutations in the CHD2 gene in eyelid myoclonia with absences amongst a number of epilepsy syndromes (46). This further supports the hypothesis that eyelid myoclonia with absences is a separate syndrome entity.
A large, multicentric study of KIAA2022-related disorders outlined the epilepsy phenotype of affected females (97). The data are consistent with a generalized developmental and epileptic encephalopathy characterized by myoclonic–atonic epilepsy overlapping with eyelid myoclonia with absences. A considerable proportion of affected females present with prolonged seizures characterized by absence status with eyelid myoclonia (125; 103). The use of advanced neuroimaging techniques in a case with a novel NEXMIF de novo mutation presenting with recurrent absence status with eyelid myoclonia revealed structural and functional changes in the brain that can alter the clinical phenotype within specific brain networks, especially in networks physiologically involved in several visuomotor functions, including motor control of eye closure and eye movements as well as attention to visual targets (22). Notably, it is not possible to determine whether the observed morphometric alterations are primarily ascribable to the dysfunction of the NEXMIF gene, or whether the repetition of prolonged nonconvulsive status epilepticus on these regions plays a role. The Neurite Extension and Migration factor gene (NEXMIF), previously known as KIAA2022, is an X-linked gene thought to play an important role in early brain development.
In general, there are no known genes responsible for eyelid myoclonia with absences. However, in some patients diagnosed with eyelid myoclonia or an eyelid myoclonia–like phenotype, four genes could be associated with this syndrome (SYNGAP1, KIAA2022/NEXMIF, RORB, and CHD2), and three more genes (SLC2A1, NAA10, and KCNB1) present also different alterations in some patients with clinical diagnosis of the disease (69).
An Xq25 microduplication involving the whole STAG2 gene was reported in an 8-year-old boy with eyelid myoclonia and absences, mild intellectual disability, speech delay, and onset at 3 years of age, fulfilling all the electroclinical criteria of what was formally named Jeavons syndrome (51). A heterozygous mutation in the PLCB1 gene was reported in a 7-year-old female with eyelid myoclonia since birth and who was diagnosed with Jeavons syndrome, which confirms the early from birth onset (102).
From an international expert consensus panel there was a strong consensus that genetic testing, epilepsy gene panel, or whole exome sequencing should be done when one or a combination of the following factors is present: family history of epilepsy, intellectual disability, or drug-resistant epilepsy (99).
Case presentation.
Three factors are important in order for eyelid myoclonia and absences (Jeavons syndrome) to manifest clinically: (1) genetic predisposition, (2) voluntary or on command slow eye closure, and (3) light input (24; 25; 26).
In order for the genetic predisposition to be expressed with electroclinical phenomena, it needs to be provoked by voluntary or on command slow eye closure in bright light. The cortical area representing eye closure lies in the precentral gyrus adjacent to the hand area (65), which is involved in self-induced epilepsy. The “cortical factor” involved in voluntary or on command eye closure seems to be important, as passive slow eye closure in the presence of light does not induce discharges or eyelid myoclonia in a predisposed person. Similar phenomena are observed in self-induced epilepsy whereby the cortical hand area is involved, and electroclinical events are induced by voluntary or on command hand waving in the presence of light. Passive hand waving, waving the nonpreferred hand, or waving the examiner’s hand in front of the patient’s eye(s) in the presence of light does not induce discharges and clinical phenomena in a predisposed person.
The frontal eye field area, occipital cortex, and subcortical circuits involving the thalamus play an important role in the genesis and spread of electroclinical paroxysms in bright light in eyelid myoclonia with absences (26). The frontal eye field area plays a critical role in voluntary eye closure (113), triggering the occipital cortex and subcortical circuit and involving thalamocortical pathways in generating and spreading the EEG paroxysms. A study found abnormal occipital and frontal cortex activities that seemed to be related to visual sensitivity and eyelid myoclonia (49). A similar pathway is probably involved in self-induced epilepsy whereby the patient, waving his preferred hand with fingers apart in front of his eyes, triggers the occipital cortex via the hand area to generate discharges as well as a subcortical circuit involving the thalamus to spread them. These systems are not triggered when, in bright light, the examiner passively closes the patient’s eyes in eyelid myoclonia and absences or waves his hand in front of the patient’s eyes in self-induced epilepsy, but the occipital lobe can be triggered directly by flashing lights (26). The background of genetic variation, which is unique to each individual’s genome, contributes to the clinical variation (70). In contrast to eye closure, the cerebral cortex is not involved in its generation during photic blink (a brainstem reflex), as experimental ablation of the occipital cortex does not influence the response (121). Some authors believe there is a malfunction of the alpha-rhythm generator or of the magnocellular and parvocellular system in eyelid myoclonia and absences (122; 85; 87). However, alpha rhythm is produced on passive eye closure. Another intriguing feature is that some cases may manifest with features of photosensitivity and fixation-off sensitivity, which have opposing characteristics (82; 84; 61; 13).
Liu and colleagues studied the ictal and interictal epileptic activity in four patients with eyelid myoclonia with absences using EEG-fMRI (66). The main regions of activation included the thalamus, mesial frontal cortex, middle parietal lobe, temporal lobe, insula, midline structures, and cerebellum. The activation in the thalamus and cortex may be associated with generalized spike-waves in eyelid myoclonia with absences, whereas deactivation in the anterior frontal regions, parietal lobe, and cingulate gyrus might suspend the default state induced by spike-wave and slow-wave complexes. The combination of consistent patterns of deactivation and varied patterns of activation in patients with eyelid myoclonia with absences may prognosticate different types of states of consciousness in response to ictal and interictal epileptic discharges.
Vaudano and associates investigated the functional and structural brain correlates of eyelid myoclonia with absences triggered by eye closure (114). Fifteen patients with eyelid myoclonia with absences, 14 cases with idiopathic generalized epilepsies without eyelid myoclonus, and 16 healthy controls underwent an EEG-correlated fMRI and voxel-based morphometry protocol. The functional study consisted of 30-second epochs of eyes-open and eyes-closed conditions. The following EEG events were marked, and the relative fMRI maps obtained (1) eye closure times, (2) spontaneous blinking, and (3) spontaneous and eye closure-triggered spike-and-wave discharges. Within-group and between-group comparisons were performed for fMRI and voxel-based morphometry data, as appropriate. Compared to the other two groups, the eyelid myoclonia with absences group had a higher blood oxygenation level-dependent signal related to eye closure over the visual cortex, posterior thalamus, and network implicated in the motor control of eye closure, saccades, and eye pursuit movements. Additionally, increments were observed in gray matter concentration at the visual cortex and thalamic pulvinar, whereas decrements were observed at the bilateral frontal eye field area. No blood oxygenation level-dependent differences were detected when comparing the spike-wave discharges in eyelid myoclonus and absences triggered by eye closure and idiopathic generalized epilepsy. Thus, these results demonstrated altered anatomo-functional properties of the visual system in eyelid myoclonia with absence seizures. These abnormalities involve a circuit encompassing the occipital cortex and the cortical and subcortical systems physiologically involved in the motor control of eye closure and eye movements (114). These findings are consistent with a study of the possible contribution of brainstem structures in the pathophysiology of eyelid myoclonus (03).
The prevalence of eyelid myoclonia with absences among idiopathic generalized epilepsies has been reported to vary from 7.3% to 12.9% and 2.5% to 2.7% among all patients with epileptic disorders (27; 48; 24; 25; 26). The age of onset, as in childhood absence epilepsy, varies from 2 to 14 years (mean 6.5 ± 2.5 years) (25), and the female-to-male ratio varies from 1.25:1 to 3.2:1 to 4.1:1 (27; 05; 19; 25; 105; 18). Eyelid myoclonia with absences may be underdiagnosed, and the mild forms are underreported.
The only way to prevent visually provoked seizures is to avoid exposure to all possible triggers, which is increasingly difficult in today’s technology-rich environment (28). Mitigating triggering factors as much as possible, reducing underlying causes, assuring compliance, and avoiding sodium-channel blocker antiepileptic drugs will help prevent seizures from happening. Early correct diagnosis using appropriate antiseizure medication at an optimum daily dose, taking into consideration the risk-benefit ratio, will contribute to better outcome. Dark lenses, particularly blue or dark cobalt blue lenses (Z1), will protect against the light trigger (28). Early diagnosis and treatment of comorbidities will also contribute to a better quality of life.
Misdiagnosis and underdiagnosis is common among the general population and among physicians. Patients with eyelid myoclonia and those who make grimaces to avoid eye closure phenomena are usually referred to psychologists or psychiatrics for tics or mannerisms.
In children, and in some adults, eyelid trembling or fluttering is often seen on eye closure and should be differentiated from mild forms of eyelid myoclonia and absences by EEG findings. Transient or chronic tics are common in childhood, particularly in males. There is a genetic and clinical heterogeneity. Motor manifestations are stereotypical, involuntary, sudden, inappropriate, nonprepositional, absurd, irresistible, and of variable intensity (24).
If seen once, the characteristic eyelid myoclonia and absences occurring immediately after eye closure will never be forgotten or confused with other conditions.
Structural, metabolic, and genetic epilepsies. Eyelid myoclonia with or without absences may be a seizure symptom in structural, metabolic, and genetic epilepsies, including Dravet syndrome, ring chromosome 20 syndrome, l-2 hydroxyglutaric aciduria, SYNGAP1-associated intellectual disability and epilepsy, KCNB1 gene mutation, and KIAA2022-related disorders (37; 72; 112; 76; 73; 115; 11; 68; 117; 118; 97). Diagnostic confusion between the patients who exhibit ictal eyelid myoclonia and those suffering from eyelid myoclonia with absences is rarely a problem based on the unique and pathognomonic electroclinical characteristics of the syndrome. Focal EEG abnormalities are common in eyelid myoclonia and absences, as in any other idiopathic generalized epilepsy, but they are likely to indicate an underlying structural abnormality when severe or persistent. In structural, metabolic, and genetic cases, eyelid myoclonia may be an inconstant ictal feature and may be associated with seizures, both of variable duration and of different types, such as atypical absences and tonic, atonic, or focal seizures. Seizure activation caused by eye closure in structural, metabolic, and genetic epilepsy cases may be rarer than in eyelid myoclonia with absences (41; 40), particularly in voluntary or on command eye closure combined with the electroclinical characteristics seen during hyperventilation and photic stimulation.
In a retrospective study, Capovilla and colleagues described 18 patients with eyelid myoclonia who also had impairment of intellectual functions and fast generalized polyspikes and polyspike and waves on EEG (18). All patients were photosensitive, highly pharmacoresistant, and had generalized tonic-clonic seizures that were mostly nocturnal.
Idiopathic generalized epilepsies with absences. Sensitivity to eye closure is also seen in juvenile absence epilepsy, juvenile myoclonic epilepsy, generalized epilepsy with tonic-clonic seizures, and idiopathic occipital lobe epilepsy. In idiopathic generalized epilepsies with absences, eyelid myoclonia should be differentiated from eyelid myoclonia with absences, which is triggered on voluntary or on command eye closure. A defining feature of photosensitivity in eyelid myoclonia with absences that distinguishes it from other idiopathic generalized epilepsy syndromes is that patients are sensitive to both flickering and nonflickering bright light (116). In a study of 90 cases with idiopathic generalized epilepsy with typical absence seizures either alone or with myoclonic jerks, generalized tonic-clonic seizures, or both, 39 (43.3%) had eyelid or eye-related ictal clinical manifestations. Only five of the cases (5.6%) had ictal manifestations similar to those occurring in eyelid myoclonia with absences (85). In addition, only one of those five was photosensitive, and another one experienced absences provoked by eye closure. Conversely, 20 patients (22.2%) had clinical or video-EEG-documented photosensitivity, but only five of them had eyelid and eye-related ictal clinical manifestations during the absences. Two patients had random eyelid blinking, which is strikingly different from eyelid myoclonia. Two patients had fast rhythmic eyelid fluttering. One patient had eyelid myoclonia with absence-like manifestations. Symptoms often overlapped in the same patient and even for the same seizure.
In certain myoclonic epilepsies, the eyes may open and stare, or the eyelids may even blink, but they do not retract and jerk as in eyelid myoclonia and absences (24). An overlap between eyelid myoclonia with absences and juvenile myoclonic epilepsy exists whereby myoclonic jerks appear as the presenting symptom; during a video-EEG recording, jerks are recorded immediately after eye closure and simultaneously with eyelid myoclonia, particularly during intermittent photic stimulation (24; 25). The coexistence of the two syndromes in the same patient has also been reported in other studies (19).
In a cohort of 50 children with eyelid myoclonia with absences, myoclonic jerks were recorded in 34% of cases, and massive myoclonias were mainly recorded during intermittent photic stimulation (24; 25). In rare cases, persistent photic stimulation may lead to a generalized tonic-clonic seizure. In a study by Kim and colleagues, even massive myoclonias were recorded among cases with eyelid myoclonia and absences having sporadic generalized tonic-clonic seizures (58). In another study, myoclonic jerks were considered an exclusion criterion (106). In an adult cohort, myoclonic jerks were recorded in 54.5% (48).
The eye closure sensitivity seen in eyelid myoclonia with absences should be differentiated from the fixation-off sensitivity characterized by posterior or generalized paroxysms that occur after closing the eyes, which last for as long as the eyes are closed (13). In eyelid myoclonia with absences, few focal abnormalities, frontal or occipital, were reported in a study (76). In another study, frontal predominance was seen in males, and occipital in females (120).
In eyelid myoclonia with absences, the eye closure period starts immediately after closing the eyes and lasts only up to 3 seconds. In the closed eye phenomenon, the period lasts longer than 3 seconds and persists as long as the eyes remain closed (126). As with early-onset absence epilepsies (23), early-onset Jeavons syndrome (24; 25; 19) has a worse prognosis regarding response to treatment and cognitive performance.
Eyelid flickering or fluttering has been reported in other types of idiopathic generalized epilepsies with absences (88; 40), symptomatic absence epilepsy (86), fixation-off sensitive epilepsy (82), and even benign myoclonic epilepsy of infancy (36). In idiopathic childhood absence epilepsy, the absence seizures are not an eye closure phenomenon and usually last longer.
Forced eyelid closure and eyelid blinking is also an ictal clinical symptom in focal seizures described in both symptomatic and idiopathic occipital epilepsy. In idiopathic occipital epilepsies, some forced eyelid closure or blinking may occur as an ictal event or herald a secondary generalized seizure (124; 81). In these cases, slow spike-wave complexes appear on eye closure in the posterior regions and continue in long runs for as long as the eyes remain closed. Eyelid flutter may be observed, but never eyelid contraction and jerking, and a partial or complete attenuation of the discharges is observed on eye opening. Generalized polyspike-wave discharges do not characterize occipital epilepsies, and the spike of the spike-wave component is smoother, as it is in all forms of benign focal epilepsies (24). Eyelid myoclonia alone can also be observed in certain symptomatic and unknown (cryptogenic) epilepsies. However, the characteristic electroclinical events of eyelid myoclonia with absences do not exist, and the associated developmental delay, neurologic deficit, abnormal MRI, and slow background EEG can easily differentiate them (40). In eyelid myoclonia with absences, the characteristic eyelid myoclonia and EEG-related discharges following eye closure, combined with photosensitivity, leave no room for diagnostic error (83; 84). Eyelid myoclonia with absences also appears to be homogeneous in people of different races and ethnicities (127).
Nonepileptic paroxysmal eyelid movements consisting of eyelid closure, upturning of the eyes, and rapid eyelid flutter have been described in patients with generalized photosensitive epilepsy and eyelid myoclonia (16; 14).
Blinking, which is a brainstem reflex, does not induce electroclinical events in patients with eyelid myoclonia with absences (24; 25).
Habitual self-induction of ictal eyelid myoclonia and absences is a rare phenomenon observed in some untreated or incorrectly treated cases, or those with borderline IQ, as well as in some early-onset cases in which the genetic predisposition is “marked.”
Self-induced epilepsy (Sunflower syndrome). Self-induced epilepsy (Sunflower syndrome) is a rare reflex photosensitive epilepsy. This self-induced epilepsy is considered a subgroup of epilepsy with eyelid myoclonia, termed “epilepsy with eyelid myoclonia with prominent photic induction” (101). Typically, the patient looks at the sun or a bright light source and rapidly waves one hand, with fingers apart, across their eyes (04). The hand waving episodes are associated with generalized spike-and-wave discharges and +/− polyspike-and-waves ranging from 3 to 4 Hz on EEG. Generalized discharges are also elicited during hyperventilation and intermittent photic stimulation (07). Seizures include eyelid flutter with or without absence seizures. Eye closure, particularly during intermittent photic stimulation, may be followed by eye opening, staring, and head jerking. The myoclonic jerks invariably involve the waving hand and head, which jerk in a similar fashion. Involvement of the lower extremities in self-induced epilepsy is more frequent than in eyelid myoclonia and absences (24). Generalized tonic-clonic seizures are rare in self-induced epilepsy but are more frequent in cases of lower IQ through the extensive use of trigger factors during long periods of boredom.
In a study of 24 cases (18 females), all patients presented with hand-waving episodes (06). The average age of onset was 6 years old, and the most prevalent symptom was an attraction to light and possible absence seizures. A 15-year-old girl was reported to have had a generalized tonic-clonic seizure following rapid hand movements in front of her eyes while staring at the sun (80). The patient had a history of multiple admissions to the emergency department due to similar events since the age of 8. Most occurrences were associated with episodes of frustration. Sunflower syndrome appears to be pharmacoresistant for the majority of patients (29; 64). In Sunflower syndrome, as in other idiopathic generalized epilepsies, some genetic and phenotypic variability exists.
If untreated or drug resistant, patients with eyelid myoclonia with absences close their eyes in bright light in order to avoid light disturbance, thereby falling into the trap of inducing discharges and clinical phenomena. This habitual behavior may be repeated in situations of boredom and anxiety. The majority of patients with only educational difficulties or discrete cognitive impairment refer to their eyelid jerking as a nuisance or a disturbing and embarrassing phenomenon that they are unable to control under certain circumstances. They are relieved when therapy is successful and show good compliance (24).
There are some similarities and differences between eyelid myoclonia and absences on voluntary or on command eye closure and self-induced epilepsy triggered by waving outstretched fingers in front of the eyes in the presence of lights (Table 1).
|
• Both syndromes are hereditary photosensitive epilepsies. | ||
|
• Clinical heterogeneity and variability in intelligence exist in both syndromes. | ||
|
• In order to manifest, both syndromes need the coexistence of three factors: | ||
|
-- genetic predisposition | ||
|
-- voluntary or on command eye closure or hand waving | ||
|
-- the presence of light; bright sunlight triggers more pronounced symptoms. | ||
|
• In both syndromes, no symptoms are triggered in total darkness. | ||
|
• In eyelid myoclonia and absences, passive eye closure or closing one eye in bright light triggers no symptoms. In self-induced epilepsy, hand waving or waving the nonpreferred hand, or even the examiner’s hand, in front of the eyes in bright light triggers no symptoms. | ||
|
• Females predominate in eyelid myoclonia with absences, and males predominate in self-induced epilepsy. | ||
|
• The eye closure and hand waving brain areas are adjacent. | ||
|
• If untreated, mistreated, drug resistant, misdiagnosed, or borderline low IQ, self-induced cases invariably provoke seizures; however, only a few cases with eyelid myoclonia and absences do. | ||
The cortical area representing eye closure lies in the precentral area adjacent to the hand area (65), and the topography of physiological networks involved follows the posterior-to-anterior trajectory of brain development, reflecting age-related changes in brain excitability (59). Light is needed to unbalance the genetically predisposed occipital cortex triggered either by voluntary or on command eye closure in eyelid myoclonia or the preferred hand waving in front of the patient’s eyes in self-induced epilepsy. The cortical factor involved in voluntary or on command eye closure or hand waving seems important as passive eye closure or hand waving in the presence of light does not induce electroclinical phenomena in the predisposed person. Further, voluntary or on command closing of one eye while looking at a light source does not trigger electroclinical symptoms.
In addition to the appropriate antiepileptic drugs, modifying bright light, the main triggering factor, by wearing dark lenses is advisable in patients with self-induced seizures. Blue or filtered lenses, eg, a dark blue lens named “Z1,” are effective (28).
In view of reports implicating slow eye closure in self-induction (33; 10), Panayiotopoulos and colleagues (87) extensively interviewed and studied video-EEG of 17 adult patients with eyelid myoclonia with absences. None of the 15 patients who were admitted were suspected of self-induced seizures. On the contrary, they considered eyelid myoclonia as a socially embarrassing condition. They were relieved when the seizures improved with medication, and they showed excellent compliance. Although other types of seizures were controlled in most of the patients, the eyelid myoclonia continued; however, it was less severe and frequent than before appropriate treatment began. This is contrary to self-induction, in which eyelid myoclonia should be more forceful after treatment if its purpose was to induce seizures. The remaining two patients were suspected of self-induction. One of the patients had frequent slow eye closure EEG abnormalities, but she never admitted self-induction. She insisted “I do not know when I am doing it…It gives me no pleasure, and it is a social embarrassment.” The other patient admitted that she was occasionally doing it voluntarily but only in rare circumstances to relax her eyes when they were strained, sore, and stung. There have been incidences “I had walked into a pole, or into a car and I did not do that on purpose.”
Eyelid manifestations in normal people. With the possible exception of violent myoclonic jerks in eyelid myoclonia, all other eyelid symptoms during absence seizures are manifested by normal people in their everyday life. The eyes and the eyelids are the most sensitive and expressive parts of our body.
Some authors reached the following conclusions on observing the behavior of a few people during TV interviews, round table discussions, and debates (85). Repetitive spontaneous blinks similar to those described in self-induced photosensitive epilepsy increased significantly during moments of tension, either at the beginning of an utterance (like a breath before starting a sentence) or at the end (like a relief). Slow and sustained eye closure was rarely manifested, and, less frequently, eyes were wide open with a cessation of spontaneous blinks. Thus, we have a simple movement that is under voluntary, automatic, reflex, emotional, and autonomic control (92).
da Conceicao and colleagues analyzed the characteristics of blinking and eye closure in 20 patients with eyelid myoclonia by video-EEG (30). Eyelid myoclonia occurred spontaneously while awake in 18 patients, on eye closure in 10 patients, and during intermittent photic stimulation in one patient. Eyelid myoclonia assumed the form of flicker, flutter, or jerk and was accompanied by generalized discharges, spiky posterior alpha rhythm, theta rhythm, or the absence of any EEG abnormality. Analysis of the characteristics of blinking had no statistical differences between patients and healthy subjects. The rate of blinks and eyelid myoclonia increased during speech and decreased during reading. Eyelid myoclonia never occurred during blinking or in the dark.
Eyelid myoclonia are myoclonic jerks of the eyelids and upward deviation of the eyes, often precipitated by closing the eyes or by light. Eyelid myoclonia can be associated with absences but can also be motor seizures without a corresponding absence, making them difficult to categorize. The 2017 classification groups them with nonmotor (absence) seizures, which may seem counterintuitive, but the myoclonia in this instance is meant to link with absence rather than with nonmotor (44; 43).
Eyelid myoclonia can only rarely be seen in typical absence seizures of idiopathic generalized epilepsy other than eyelid myoclonia with absences. In a study of 60 such patients with video-EEG recorded absence seizures, only five had eyelid myoclonias (85). Of these five patients, only one was also photosensitive, and only one experienced seizures precipitated by eye closure.
Absence status epilepticus with eyelid myoclonia. Continuous clusters of prolonged seizures of eyelid myoclonia with absences may occur as the result of accumulating precipitating factors, discontinuation, or inappropriate treatment. They are more likely to occur on awakening (98; 02; 119; 08; 83; 84; 62).
A 12-year-old girl presented with a history of two distinct episodes of status epilepticus (63). Her CNS examination was within normal limits. The detailed history disclosed multiple episodes of jerky movement of the eyes followed by vacant spells lasting for a few seconds, which was noted from the age of 3.5 years but treated as nonsignificant. The EEG was abnormal, with generalized spike-and-wave epileptic activity with eye closure sensitivity diagnostic of Jeavons syndrome. In another case, the diagnosis of eyelid myoclonus with myoclonus status was made on the basis of history and video documentation recorded by family members (57). It is distinguished by myoclonia of the eyelids that develops right after the eyes close and is linked to generalized EEG paroxysms.
Eyelid myoclonia with absences in unknown (cryptogenic) or symptomatic generalized epilepsies. Eyelid phenomena are commonly seen during nonconvulsive seizures in children with unknown (cryptogenic) and symptomatic generalized epilepsies. These include eyelid blinking and flutter. True eyelid myoclonia is less common (40; 82).
In a report, two female pediatric patients with probable genetic cryptogenic epilepsy presented with eyelid myoclonia with prominent myoclonic seizures, atonic components on video-EEG, and cognitive impairment (35).
|
• The diagnosis is easy based on the history; observation of the patient; and detailed sleep-awake video-EEG, with correct technique and assessment during photic stimulation (54; 24; 56). Video-EEG is the single most important procedure to diagnose and elucidate the unique electroclinical characteristics of eyelid myoclonia with absences. During drowsiness, hyperventilation, and intermittent photic stimulation, an exacerbation of clinical and EEG events is seen (25). Neuroimaging is usually done when intellectual disability is present and in atypical and drug-resistant cases. Genetic testing, an epilepsy gene panel or whole exome sequencing is also performed in specific cases when intellectual disability, drug resistance epilepsy, or family history of epilepsy is present. | |
|
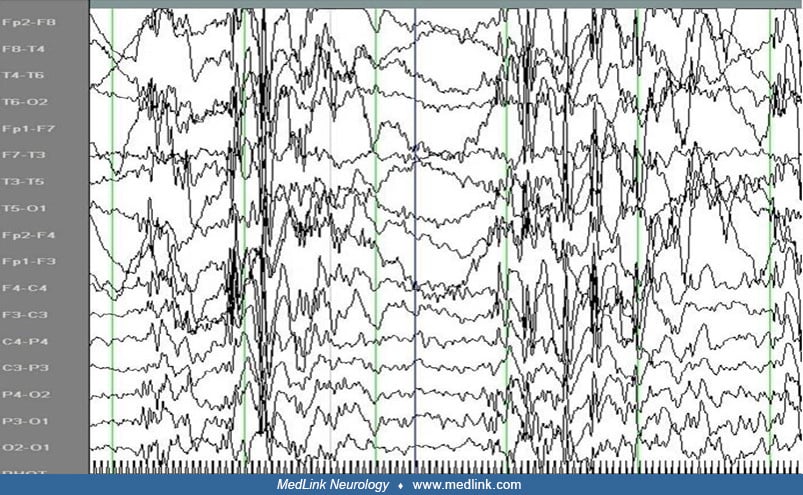
• Interictal EEG. EEG is dominated with high-amplitude discharges of spike-and-slow waves at 3 to 6 Hz. These are brief (1 to 5 seconds) and are commonly associated with clinical manifestations of eyelid myoclonia of varying severity. They occasionally appear simultaneously with impairment of cognition. They often occur immediately (within 0.5 to 2 seconds) after voluntary or on command eye closure in an illuminated recording room. They are eliminated in total darkness. Photoparoxysmal responses are recorded from all untreated young patients and may be absent in older patients on medication. Photosensitivity and fixation-off sensitivity may occur together (82). |
A study emphasized a high incidence of (1) focal interictal epileptiform discharges from the posterior head region and (2) predominant focal posterior ictal epileptiform discharges preceding generalized epileptiform discharges (116). Focal frontal spikes may sometimes precede the generalized discharges (107). According to a report from China, a predominantly male group had frontal predominant epileptiform discharges, eyelid myoclonia, and eyes rolling up, and a predominantly female group had occipital predominant epileptiform discharges with eyelid myoclonia alone (120).
Sleep EEG may be normal or may show generalized spike-wave discharges, focal spikes, or spike-and-wave complexes in the frontal regions. The generalized discharge of polyspike-slow waves during sleep tends to be of longer duration and fragmented. In a few cases, a slight tremor of the eyelids or an opening and closing of the eyes is observed during the discharge. The discharges are shorter and devoid of discernible clinical manifestations of any type, even in patients who have numerous seizures during the alert state. Sleep EEG patterns are normal. EEG and clinical manifestations deteriorate consistently after awakening.
Ictal EEG. Ictal EEG accompaniments of eyelid myoclonia with absences are generalized discharges of mainly polyspikes and polyspike-slow waves at a frequency of 3 to 6 Hz (usually more than 4 Hz) and a duration of 3 to 6 seconds (typically around 3 seconds and seldom more than 5 seconds).
Eyelid myoclonia with absences is a lifelong disorder, and its prognosis is similar to that of juvenile myoclonic epilepsy with photosensitivity. Appropriate treatment usually results in significant reduction of seizures and prevention of eyelid myoclonia status epilepticus, as well as generalized tonic-clonic seizures.
Lifelong treatment with medication may be necessary for patients with eyelid myoclonia with or without absences. In the absence of controlled therapeutic trials, it is not possible to draw scientifically valued conclusions about the most effective approach to the drug treatment of eyelid myoclonia with or without absences.
Eyelid myoclonia with absences is difficult to treat but responds better to valproate; long-acting valproate once daily improves compliance. In 1982, Covanis and colleagues reported that monotherapy with sodium valproate was successful in 53% to 76% of idiopathic generalized epilepsies (29). The worst results were seen in eyelid myoclonia with absences and the best in pure photosensitive epilepsy. About 20 years later, the response was reported in 74% to 86%, respectively. Based on 50 cases, the increased response of eyelid myoclonia with absences to valproate, from 53% to 74%, was attributed to early diagnosis and treatment. Valproate remains the most effective treatment for photosensitive epilepsies (29; 59) and should be considered early. For nonresponders to monotherapy with sodium valproate, a combination of sodium valproate and ethosuximide is considered to be the most effective regimen. However, clonazepam, which is highly effective in myoclonic jerks, may be a valid option. Small doses of lamotrigine added to sodium valproate may result in dramatic improvement because of their possible pharmacodynamic interaction (42). Lamotrigine alone may exaggerate myoclonic jerks.
Women with epilepsy with eyelid myoclonia taking valproate must be aware of the risk of polycystic ovary syndrome and monitor their menstrual cycles. A 26-year-old female was given valproate for generalized seizures since the age of 12 years and then developed polycystic ovaries. Fifteen months after valproate withdrawal polycystic ovary syndrome was cured, but her epilepsy became intractable. From the history, a video-EEG reevaluation, 15 years after onset, put diagnosis of epilepsy with eyelid myoclonia. Vagus nerve stimulation achieved greater than 50% seizure reduction in a short term follow-up (108).
An international panel of experts for the management of epilepsy with eyelid myoclonia proposed a strong consensus for valproic acid as the first-line treatment, with levetiracetam or lamotrigine as preferable alternatives for women of childbearing age. There was a moderate consensus that ethosuximide and clobazam are also efficacious. There was a strong consensus to avoid sodium channel-blocking medications, except for lamotrigine, as they may exacerbate the syndrome (100).
However, in women with epilepsy who are in childbearing age, safe pregnancies have been a great concern, particularly in those taking valproate. Safety issues include the risk for obstetrical and perinatal complications, offspring outcomes, as well as maternal seizure control (111). Valproate is associated with greater risk of teratogenic effects such as major congenital malformations and adverse neurodevelopmental outcomes including autism spectrum disorders and intellectual disabilities. Valproate may be considered as an appropriate treatment option for the generalized epilepsies where it is more effective than other drugs, in female children with epilepsies that have a high likelihood of remission and treatment withdrawal before puberty, in severe nature epilepsies, or the patient has concurrent severe disabilities, which means future pregnancy is extremely unlikely (110). The U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have provided guidelines with the following recommendations, in brief, for women with epilepsy on valproate: valproate must not be used during pregnancy unless is difficult to stop, if other treatments are ineffective or not tolerated, and the conditions of the new pregnancy prevention program are met, such as effective contraception throughout treatment and counselling patients about the risks of valproate treatment.
Levetiracetam may be effective because of its anti-myoclonic and anti-photosensitive properties (105; 84; 89). In a prospective clinical trial, it was found that levetiracetam was most effective if given at a dose of 50 to 60 mg/kg/day (105; 89). Exacerbation of eyelid myoclonia in two cases of eyelid myoclonia with absences was associated with cannabidiol use and resolved after cannabidiol discontinuation (128). In another publication, a patient with eyelid myoclonia with absences showed significantly higher impulsivity compared to healthy controls and those with juvenile myoclonic epilepsy, and impulsivity was higher in those treated with levetiracetam (67).
Perampanel has also demonstrated efficacy and safety in generalized tonic-clonic seizures among patients with idiopathic generalized epilepsy and does not seem to exacerbate absence seizures (12).
Carbamazepine, oxcarbazepine (71), gabapentin, phenytoin, pregabalin, tiagabine, and vigabatrin are contraindicated (83; 84).
Patients who deliberately use visual stimulation to induce either overt seizures or ‘‘subclinical’’ epileptiform EEG discharges are very resistant to valproate and to any combination of antiepileptic drugs, even if they are compliant (25).
Responsive neurostimulation bilaterally targeting the centromedian and ventrolateral region of the thalamus was given in a patient diagnosed with eyelid myoclonia with absences who was refractory to medication (60). Responsive neurostimulation decreased daily absence seizures from a mean of 60 to 10 or more and maintained the patient's level of consciousness during the occurring episodes.
Nonpharmacological treatments used for photosensitive patients should be employed in eyelid myoclonia with absences when photosensitivity persists (123; 29). Wearing special tinted glasses (123; 29) or the commercially available blue Z1 lenses may be beneficial (17; 28). Self-induced seizures might be modifiable by psychiatric treatment.
In general, by choosing the correct antiepileptic medications at an appropriate daily dose taking into consideration the risk-benefit ratio and recognizing comorbidities for early intervention contributes to better management. Sodium valproate has proven to be successful for this type of seizure, either as monotherapy or combined with other appropriate antiepileptic drugs. Taking into consideration dose-related teratogenicity, it should be avoided as a first choice in adolescent females. Special care should be given to females on valproate who intend to become pregnant or are pregnant; the daily dose of sodium valproate should be based on a careful risk-benefit decision (110). There is an urgent need for the development of up-to-date, globally applicable recommendations (109).
Appropriate and early treatment usually results in a significant reduction of seizures and prevention of eyelid myoclonia status epilepticus, as well as generalized tonic-clonic seizures and better outcome.
Photosensitivity tends to disappear in middle age. In some cases, a mild eyelid flutter in association, or not, with theta-beta discharges on eye closure persists. Eyelid movements that are not associated with EEG discharges on eye closure constitute a habitual tick-like behavior and are observed in patients who never received treatment or did not show complete response to treatment. This behavior may continue for a few years after eyelid myoclonia, and absences have completely vanished (25).
Cases that start under the age of 3 years are, as a rule, drug resistant and have moderate to severe educational problems requiring remedial teaching. Electroclinical features of early-onset cases, including photosensitivity, gradually disappear before puberty, and the child starts showing signs of educational improvement. In addition, cases that are misdiagnosed or are inappropriately treated for many years, or those that show noncompliance, and associated comorbidities that are not diagnosed or treated early have a worse prognosis. In an electroclinical study of 40 patients with eyelid myoclonia with absences, all had absences over the course of the disease (childhood to adulthood) (77). Intellectual disability and psychiatric disorders were reported in 35% and 45%, respectively.
In a multicenter retrospective study of 172 patients with eyelid myoclonia with absences in which the median age of onset was 7 years and the median follow-up was 14 years, the electroclinical endophenotypes and long-term seizure outcome were investigated (21). Sixty-six patients (38.4%) displayed a nonremission pattern, whereas remission and relapse patterns were encountered in 56 (32.6%) and 50 (29.1%) participants, respectively. They identified two clusters of 86 patients each. Cluster 1, the eyelid myoclonia–only cluster, was characterized by a higher rate of seizure remission and more favorable neuropsychiatric outcome. Cluster 2, defined as eyelid myoclonia–plus, was characterized by an earlier age at epilepsy onset, higher rate of intellectual disability, eyelid myoclonia status epilepticus, generalized paroxysmal fast activity, self-induced seizures, febrile seizures, and poor antiseizure response. Early-onset epilepsy was the most relevant prognostic factor for poor treatment response.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Thanos Covanis MD DCH PhD
Dr. Covanis of Childrens’ Hospital Agia Sophia in Athens, Greece has no relevant financial relationship to disclose.
See Profile
Solomon L Moshé MD
Dr. Moshé of Albert Einstein College of Medicine has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Epilepsy & Seizures
Jan. 20, 2025
Epilepsy & Seizures
Jan. 09, 2025
Epilepsy & Seizures
Jan. 09, 2025
Epilepsy & Seizures
Dec. 23, 2024
Epilepsy & Seizures
Dec. 19, 2024
General Child Neurology
Dec. 10, 2024
Epilepsy & Seizures
Dec. 03, 2024
Epilepsy & Seizures
Dec. 03, 2024