Epilepsy & Seizures
Tonic status epilepticus
Jan. 20, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Neonatal brachial plexus palsy can be a debilitating injury that leads to long-term disability in the infant. Although the majority of cases do recover full function of their arm, others must undergo surgery or other treatments to improve function. This article describes the pathology and anatomy of brachial plexus palsy, provides tips to examine an affected patient, and reviews the available treatment options.
|
• The most common brachial plexus palsy involves the upper roots, C5 and C6, and is called Erb palsy. | |
|
• The spontaneous recovery rate is 60%, and some children suffer permanent impairment. | |
|
• Surgical treatment is usually offered between 3 to 6 months of age for primary repair; otherwise, patients can undergo secondary procedures around 12 to 18 months of age. | |
|
• A multidisciplinary approach with the pediatrician, physical and occupational therapists, and the surgeon is very helpful when treating an infant with brachial plexus palsy. |
Several authors have suggested that German artist Albrecht Dürer (1471–1528) painted a case of Erb palsy in his Haller Madonna (before 1505), in part because of the internal rotation and pronation of the left arm, with accentuation of the skin folds of the anterior axillary region and drooping of the left shoulder (92; 139; 146). A suggested alternative diagnosis is pseudoparalysis from a fractured clavicle or humerus, which can resemble a brachial plexus palsy (139), although clavicular fractures can coexist with neonatal brachial plexopathies in about 10% of cases of obstetric brachial plexus palsy. However, despite the common modern practice of assigning putative diagnoses to centuries-old art, the child is holding a piece of fruit in his left hand, with the same posture that Dürer painted Eve holding a piece of fruit in her left hand (139). A child with an Erb palsy would be very unlikely to hold a piece of fruit in the pathologic hand. The posture of the child is typical of the Mannerism style of northern European paintings at the time, which featured hyper-idealization, exaggerated poses, distorted human forms, and awkward movement.
William Smellie. Neonates who have neurologic deficits have been observed since the time of the ancient Greeks and Hippocrates (76). Brachial plexus palsy related to the birth process, “obstetric brachial palsy,” was described by Scottish obstetrician William Smellie (1697–1763) in a textbook originally published in 1754 titled A sett of anatomical tables, with explanations, and an abridgment, of the practice of midwifery (158; 160; 161; 162; 111; 134; 150; 157).
Smellie was highly regarded for his obstetrical skills and for his monographs and atlas showing elaborate depictions of the development of the fetus, the birth process, and obstetric problems (158; 160; 161; 159; 162). Smellie is particularly known for his incredible illustrations of pregnant women and fetuses, drawn from cadavers. Some of his illustrations vividly show the circumstances that often led to obstetrical brachial plexus palsies in neonates. However, the large number of pregnant cadavers that Smellie was able to amass for his huge atlas led to recent allegations that he and the Hunter brothers encouraged or arranged for the murder of pregnant women to complete their projects (150).
Traction on the arm at this point can lead to severe traction on the brachial plexus and cervical nerve roots. (Source: Smellie W. A treatise on the theory and practice of midwifery, to which is added, a set of anatomical plate...
(Source: Smellie W. A treatise on the theory and practice of midwifery, to which is added, a set of anatomical plates, exhibiting the various cases that occur in practice, accurately engraved, with explanations. London: Alexand...
Although Smellie is frequently credited with describing obstetrical brachial plexus palsy, his description was quite limited. He described, in rather vague terms, transient bilateral arm weakness in a neonate following a complicated delivery that occurred in 1746 (161). The initial presentation was breech, but this was converted to a face presentation that resulted in the arrest of labor. Smellie was able to deliver the child with forceps. As Smellie later recounted, "The long compression had rendered the arms paralytic for several days, though this misfortune was soon remedied by friction and embrocations [a liquid used for rubbing on the body to relieve pain from sprains and strains]" (161).
Wilhelm Heinrich Erb. German neurologist and neurophysiologist Wilhelm Heinrich Erb (1840–1921) first compared neonatal brachial plexus palsy with that found in adults and concluded that it involved the upper roots (184; 147).
Guillaume-Benjamin-Amand Duchenne (de Boulogne). The term “Duchenne-Erb palsy” was coined because French neurologist Guillaume-Benjamin-Amand Duchenne (de Boulogne) (1806–1875) received credit for describing the brachial plexus palsy following delivery of affected newborns (46; 22; 142; 86; 64; 129; 143; 147).
In 1862, Duchenne published a pioneering collection of photographic images of patients with various neuromuscular diseases, including one with an Erb (upper plexus) palsy (47). Duchenne also recognized an association with clavicular fractures, subacromial dislocations, and ipsilateral brachial plexus injuries.
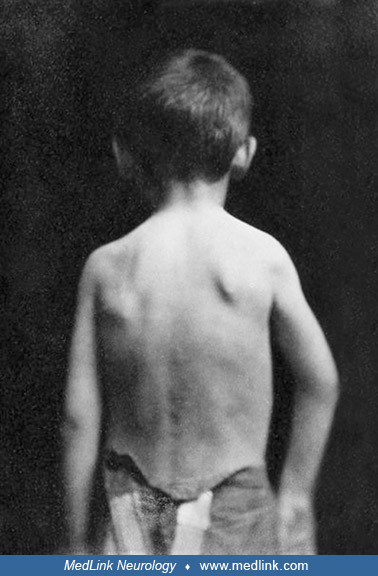
As described by Duchenne: Posterior and external dislocation of the shoulder (subacromial dislocation), dating from birth, in a 6-year-old boy, characterized: (1) by a relief located below the posterior angle of the acromion, f...
In 1872, Duchenne further described the child that he had photographed in 1857. A 6-year-old boy was presented to Duchenne for treatment of congenital right arm weakness (46).
|
In March 1857, a young boy named Théophile Bigot, aged 6, was presented to me to be treated for a congenital paralysis of the upper right limb. The movements of the latter were, in fact, so hampered since his birth that he could not use them. All muscles responded normally to electrical excitation. His right shoulder was deformed; the attitude of the arm on this side was abnormal (see the figure drawn from the photograph I took of it). One noticed on the posterior face of the stump of the shoulder, a little below the posterior angle of the acromion, a rounded relief that indicated, in this point, the presence of the head of the humerus, which, moreover, one recognized perfectly by touch. Anteriorly, the shoulder stump presented a slight subacromial depression, but without apparent relief of the coracoid process, and the head of the humerus was no longer found in its normal position. This head of the humerus appeared to be straddling the posterior edge of the glenoid cavity. It was certainly not in the infraspinatus fossa; it was difficult to explain it, but what was indisputable was that it had remained thus incomplete for 6 years. The elbow, carried a little forward, was set aside from the body and could not be brought closer to it; attempts to obtain it caused pain. The humerus was kept in rotation inwards [internally rotated], and one could not mechanically impart to it the slightest movement in the opposite direction without making the child cry out. The forearm was a little flexed on the arm, without it being possible to extend it completely. The voluntary movements of the arm were weak and limited like those of the forearm. | |
|
(46), translation by Dr. Douglas J Lanska |
(Source: Duchenne [de Boulogne] GB. Paralysies obstétricales infantiles des membres supérieurs avec ou sans fractures, luxations ou autres complications. In: De l'électrisation localisée et de son application à la physiologie, ...
Duchenne noted that three other children were referred at around the same time with the same deformity of the shoulder and with the same disturbances in the movements of the arm on the shoulder. He recognized the characteristic signs of scapulohumeral dislocation in all these children. The cause of this dislocation appeared to be identical in all these cases and, in particular, to be the result of extreme force being applied during delivery:
|
The parents of the children said in fact that their birth had been laborious—that, to extract them, [the midwife or physician] had to exercise long and violent pulls, using a finger or a hook passed under one of the armpits, and that the limb exposed to these pulls had been deprived of movements after their birth. It was precisely on this side that the dislocation existed, the production of which is very well explained by the violence exerted on the armpit. | |
|
(46), translation by Dr. Douglas J Lanska |
With more extensive obstetric brachial plexus palsies, Duchenne also noted the effects of the weakness on the posture of the arm and hand, the development of contractures, and the changes in strength over time. One child was born in "dire circumstances" with a shoulder presentation—a malpresentation in which the fetus is in a transverse lie (ie, its vertebral column is perpendicular to that of the mother) so that the leading part (the part that first enters the birth canal) is an arm, a shoulder, or the trunk. In addition, the umbilical cord was wrapped around his neck, and the delivery was "long and arduous." He sustained perinatal asphyxia and was "hardly brought back to life." As further evidence of birth trauma, he had a fractured ulna near the elbow joint. After his birth, he did not move his upper right arm. Initially, Duchenne noted no clear difference in the appearance of the right arm and hand, but in a few months, the hand gradually became deformed and less developed than the opposite arm. Duchenne concluded that, "Atrophic paralysis and deformation of the hand are the result of the lesion of some nerves involved in the fracture of the bones of the forearm during the maneuver of childbirth" (46), translation by Dr. Douglas J Lanska.
Duchenne applied faradic currents to the arm, and, over time, the child's hand function and appearance improved, though the child still had limited function of the arm and hand.
|
I saw .... the shape of the hand return to its normal state by the return of their tonic force. [This figure] was drawn from the photograph I made of the hand of the sick little one after his treatment. If we compare it to [the hand] photographed and then drawn during the treatment, we notice that the claw no longer exists ... that the last two phalanges have extended and that the first have flexed a little. This reestablishment of the normal shape of the hand was due to the development of the interossei. The eminences had also developed as well as the atrophied muscles of the forearm. ... [T]he movements of the upper limb had gained in strength and extent, but they had not recovered their independence. ... I was hopeful that with the help of certain gymnastic exercises prescribed by me, [he would continue to improve]. Two years later, this young boy came to show me that this hope had come true; he used that hand almost as well as the other. | |
|
(46), translation by Dr. Douglas J Lanska |
Duchenne presented one further illustration of the "deformation of the hand,” following a childhood obstetric subacromial dislocation.
|
The disorders caused, in these children, in the movements and in the attitude of the limb, by the subacromial dislocation [of the acromioclavicular joint], may well suggest the existence of a congenital cerebral palsy of the upper limb; in either case, the elevation of the arm is difficult and limited. Furthermore, the hand is pronated, and the arm internally rotated... [I]n all these children, there existed, moreover, a veritable paralysis that had been occasioned by the lesion of the brachial plexus and which was more or less complete and more or less serious. Thus, in one of them ... some muscles were atrophied or responded weakly to electrical excitation (the biceps and the anterior brachialis) or had lost their electrical contractility (flexors of the fingers and interossei). | |
|
(46), translation by Dr. Douglas J Lanska |
Augusta Klumpke. In addition, brachial plexus injury to the lower roots (C8-T1) was first described by American-born French neurologist Augusta Klumpke (1859-1927) in 1885 (95; 132; 20; 21; 64; 153; 188; 51).
Erb palsy in Kaiser Wilhelm II of Germany. In 1859 Wilhelm was born in Berlin to Victoria (or "Vicky"; 1840-1901), Princess Royal, the eldest daughter of Britain's Queen Victoria (1819-1901), and Prince Frederick William of Prussia (the future Frederick III; 1831-1888)--a marriage intended to unite the royal families of Britain and Germany. A traumatic breech birth resulted in an Erb palsy, which left Wilhelm as an adult with a withered left arm about 6 inches (15 centimeters) shorter than his right. In a letter to her mother, Queen Victoria, Vicky wrote, "The idea of his remaining a cripple haunts me." She felt a cure had to be found, and subjected Wilhelm to various bizarre procedures that served only to traumatize the boy. Beginning at 6 months of age and continuing for years, a hare was slaughtered in his presence twice a week to provide "animal baths"; the still-warm flesh of the dead hare was then tied around boy's left arm, with the hope that the vitality of the wild animal would somehow be transferred into the boy's dysfunctional arm. As the boy became more mobile, they tied his good arm behind his back thinking that this would force him to use and strengthen his weak arm, but this was of course a plan destined to fail and one that only heaped frustration and agony on the growing boy. In another letter to her mother, Queen Victoria, Vicky wrote: "It [He] gets so fretful and cross and violent and passionate that it makes me quite nervous sometimes." For most of his childhood, Wilhelm's withered arm was also subjected to electrotherapy treatments that were not only painful but that succeeded only in provoking a nervous reaction in the young boy. It was only at age 12 that the many, varied, and painful attempts to cure his disability were finally abandoned. Even then, Wilhelm's deformity was considered an embarrassment that had to be kept hidden from public view, but the deformity was, of course, still present, to his mother's shame. Vicky viewed the delivery of a less than physically perfect heir to the Prussian throne as a personal failure and, moreover, one that raised concerns about the ability of her son to thrive in the militant court atmosphere that was his destiny. In still another letter to her mother, Vicky confessed that the deformity "spoils all the pleasure and pride I should have in him." Although her rejection of her son stemmed in part from her failure to bring forth a strong male heir, no doubt compounded by the responsibility she felt (or blame she perceived) as the English mother of a German heir, it was nevertheless a quite terrible reaction by a mother toward her own son and one that Wilhelm reacted to in anger and resentment.
In most of the extant photographs and paintings, the royal photographers and painters concocted a remarkable diversity of subterfuges to obscure the left hand or to otherwise conceal its deformity (although some paintings and sculptures adopted an altogether different approach: just portray the arm and hand as if they were normal!). Photographs and paintings show Wilhelm holding a pair of white gloves in his left hand to make the arm seem longer, hiding his left hand under crossed arms, hiding his left arm behind his back, covering his left hand with his right on the hilt of a sword, putting his left hand in a pocket, holding his left hand with his right, holding a cane to give the illusion of a useful limb posed at a dignified angle, or hiding his hand and arm under a cape. There are also some officially sanctioned paintings and sculptures that portray his left arm and hand as if they were normal.
Prince Wilhelm c1871 as a 12-year-old boy in Berlin. Note the small size of his left hand, a result of his Erb palsy from obstetric trauma. The white glove is a prop, intended to suggest, by extension, a longer left arm. Despit...
Kaiser Wilhelm II in 1905. Wilhelm in dress military regalia, wearing an elaborate "eagle spike" Pickelhaube helmet. He is resting his diminutive and deformed left hand on a sword hilt and then covering it with his normal right...
The disability from obstetric brachial plexus palsy clearly affected Wilhelm’s emotional development, and seemingly caused him to over-compensate through aggressiveness and competitiveness. Instead of his life providing a bridge to strengthen the ties of Britain and German, he ultimately initiated actions that split them apart.
Surgical case series from Leon Pierce Clark and colleagues (1905–1907). In 1905, neurologist and psychiatrist Leon Pierce Clark (1870–1933), neurosurgeon Alfred S Taylor (1869–1942), and pathologist Thomas P Prout described the results of 20 dissections and many experiments on infantile cadavers as well as a series of operations on seven clinical cases, which indicated that tension (overstretching) of the nerve roots of the brachial plexus was the basis of obstetric brachial plexus palsies. In this surgical case series from the beginning of the 20th century, two of seven cases (29%) died in the perisurgical period (34). This series gives a useful perspective on the range of presentations, the operative findings, and the degree of recovery achieved at that time.
Case 1. A 25-month-old girl with complete paralysis of her left arm. She was a first child and with vertex presentation. Labor was prolonged and difficult. Instruments were used, and strong traction was exerted on the head. Complete paralysis of the left arm was noted a few days after birth. No spontaneous improvement resulted during the first 2 months after birth. After 4 months, slight flexion of the fingers and wrist was possible. Contractures contributed to the deformity. The child died 19 hours after surgery in 1903.
Case 2. A 10-year-old girl with typical "laceration" (stretch) brachial birth palsy. Typical birth palsy of a milder grade was present. She was the fourth child and with vertex presentation and marked asphyxiation after labor lasting 7 hours. "Forceps were used and great force employed in delivery." Palsy of the right arm was at once noticed. Improvement began at the end of 4 months and continued for 1 year. Slight contractures occurred in all the paralyzed muscles, producing a characteristic deformity. At operation in 1903, the fifth and sixth nerve roots were found to be damaged. A 1 cm portion was excised, and the proximal and distal ends were sutured. Marked return of muscle power began 3 months after surgery and continued for 2 years.
Case 3. An 8-year-old boy with typical "laceration" (stretch) brachial birth palsy. Obstetric birth palsy of the right arm (Erb palsy) was present. He was the third child and with vertex presentation. Labor lasted 14 hours, and instrumentation was finally used. After prolonged and forceful traction, he was born asphyxiated and with total paralysis of the right arm. During the first year, there was some slight return of power, but there was no subsequent improvement. The right arm and shoulder girdle were distinctly underdeveloped compared to the left side and in x-ray images. The shoulder was a flail joint. The elbow could not be extended more than 150 degrees. The wrist was markedly flexed and adducted (toward the ulna). The extremity was cooler than the normal one, and the hand was purple-colored. The bones on the damaged side were between 12% and 20% shorter than the corresponding bones on the opposite side. There was a pronounced posteroinferior dislocation of the shoulder. The coracoid and acromion processes were longer, more pointed, and bent more downward and forward than normal. At operation in 1903, the upper trunk of the brachial plexus was found to have been torn apart, and the torn ends were displaced and adherent to other structures with connective tissue. The damaged tissue was excised, and the ends sutured. The boy made steady but very slow progress postoperatively, and after 9 months, he was able to move his arm slightly.
Taylor and Prout presented further information on the surgical treatment of brachial birth palsy in 1907 (169). Further return of function was evident in the arm of this patient 2 years and 7 months following the first operation.
Case 4. An 8-month-old boy with typical "laceration" (stretch) brachial birth palsy of the right arm. “Typical birth palsy” was present. He was the third child and with vertex presentation. Labor was 72 hours long and was conducted by a midwife, who, when the head was born, pulled forcibly on it to deliver the shoulders, which were caught (shoulder dystocia). Two days later, paralysis of the right arm was noticed. No improvement occurred prior to operation. At operation, only the fifth and sixth cervical roots were affected near where they join to form the upper trunk of the brachial plexus. The child died 3 days after surgery.
Case 5. A 4.5-year-old boy with a mild degree of "laceration" (stretch) brachial birth palsy of the right arm. He was the second child and with vertex presentation. “Very difficult labor. Instruments used after 19 hours and 'great pulling' was employed." The right arm was paralyzed at birth. Movements began to return at the end of 3 months, but by the age of 6 months, the improvements had stopped. Paralysis, deformity, contractures, and atrophy were typical of a medium-grade birth palsy. At operation in 1904, a portion of the damaged fifth and sixth roots and the proximal portion of the upper trunk of the brachial plexus were resected and the free ends sutured. No movement was evident in C5- and C6-innervated muscles for 3 months. Slow improvement occurred thereafter, but the child was poorly cooperative with instructions, so little hope of significant further progress was expected.
Case 6. An 11-year-old girl with a mild degree of "laceration" (stretch) brachial birth palsy of the left arm. She was the first child and with vertex presentation. "Delivered by a midwife, who pulled on the head." Partial paralysis of the left arm was noticed within the first 2 days. After several months, improvement began and continued for about 2 years, appearing first in the hand muscles and then extending upward. At operation in 1904, a lesion was found in the fifth nerve root and the outer part of the junction of the fifth and sixth nerve roots (upper trunk of the brachial plexus). The damaged portion was excised and the free ends sutured. The lesion resulted from a traction injury, with rupture of the perineural sheath and hemorrhage into its substance and into the meshes of the epineurium.
Schematic representation of a rupture of the perineural sheath and hemorrrhage into its substance and into the meshes of the epineurium, resulting in the formation of a hematoma. Legend: (a) epineurium, (b) perineurium, (c) ner...
|
• Injury to the brachial plexus can be classified by the anatomic localization of the nerves affected, such as the upper, lower, or total plexus. | |
|
• Erb (or Erb-Duchenne) palsy, being the most common form of brachial plexus palsy in neonates, is caused by disruption of the upper brachial plexus nerves at cervical nerve roots 5 and 6, and possibly 7 (C5-C7). | |
|
• Clinical findings for C5-C6 palsy include shoulder muscle paralysis with an asymmetric Moro reflex, an internally rotated upper arm, an extended elbow due to flexor paralysis, a pronated forearm, and a flexed wrist. | |
|
• If C7 is also involved, the baby may have a “waiter's tip” posture with adduction and inward rotation at the shoulder, extension and pronation at the elbow, and flexion of the fingers. | |
|
• Klumpke palsy is a less common form of brachial plexus palsy in neonates and is caused by involvement of the brachial plexus at cervical roots 7 and 8 and thoracic root 1 (C7-C8, T1). | |
|
• Classic clinical signs of Klumpke palsy include a supinated forearm with a flexed wrist and fingers, a “claw hand,” and an absent grasp reflex. | |
|
• In lower brachial plexus palsy, the involvement of the sympathetic nerves from the first thoracic root, which gives rise to the superior cervical sympathetic ganglion, can result in ipsilateral Horner syndrome manifested by ipsilateral constricted pupil, upper lid ptosis, and facial anhidrosis. | |
|
• Total brachial plexus palsy is often erroneously called "Klumpke" palsy as the patient presents with a lesion of C7-T1, but total brachial plexus palsy is always associated with an upper spinal nerve lesion of varying severity. | |
|
• The phrenic nerve, arising from C3, C4, and C5 can be involved in brachial plexus palsy with resultant ipsilateral diaphragmatic paralysis, causing a decrease in thoracic space, tidal volume, and vital capacity. |
Injury to the brachial plexus can be classified by the anatomic localization of the nerves affected, such as the upper, lower, or total plexus. Erb (or Erb-Duchenne) palsy, being the most common form of brachial plexus palsy in neonates, is caused by disruption of the upper brachial plexus nerves at cervical nerve roots 5 and 6, and possibly 7 (C5–C7) (112). Clinical findings for C5-C6 palsy include shoulder muscle paralysis with an asymmetric Moro reflex, an internally rotated upper arm, an extended elbow due to flexor paralysis, a pronated forearm, and a flexed wrist (66; 83; 183). If C7 is also involved, the baby may have a “waiter's tip” posture with adduction and inward rotation at the shoulder, extension and pronation at the elbow, and flexion of the fingers (66; 183). In children with an upper plexus lesion, in addition to the motor deficits, the sensibility of the thumb and index finger is diminished, which has a significant negative impact on hand function (24; 25).
Klumpke palsy is a less common form of brachial plexus palsy in neonates and is caused by involvement of the brachial plexus at cervical roots 7 and 8 and thoracic root 1 (C7-C8, T1) (112). Classic clinical signs include a supinated forearm with a flexed wrist and fingers, a “claw hand.” These patients have absence of the grasp reflex on examination (83). In lower brachial plexus palsy, the involvement of the sympathetic nerves from the first thoracic root, which gives rise to the superior cervical sympathetic ganglion, can result in ipsilateral Horner syndrome manifested by ipsilateral constricted pupil, upper lid ptosis, and facial anhidrosis. However, total brachial plexus palsy is often called "Klumpke" palsy as the patient presents with a lesion of C7-T1, but total brachial plexus palsy is always associated with an upper spinal nerve lesion of varying severity (128). Obstetrical-induced Klumpke palsy with only a paralyzed hand is extremely rare (09).
The phrenic nerve, arising from C3, C4, and C5 can be involved in brachial plexus palsy with resultant ipsilateral diaphragmatic paralysis, causing a decrease in thoracic space, tidal volume, and vital capacity. The neonate can develop tachypnea, cyanosis, and inefficient ventilation (07; 36). If brachial plexus palsy is associated with injury to cervical spinal cord, the patient may be unable to breathe, resulting in subsequent ventilator dependence or death (36; 155).
Among newborns born vaginally by breech or cephalic presentation, those born breech are more likely to develop Erb palsy, whereas those in the cephalic group are more likely to have total brachial plexus palsy (10). Breech infants have a higher frequency of bilateral obstetrical brachial plexus palsies and concurrent phrenic nerve palsy (10). Concurrent phrenic nerve palsy in neonates with brachial plexus palsy is a strong negative prognostic indicator for spontaneous motor recovery of the brachial plexus, particularly after vertex delivery (189). In contrast, concurrent Horner syndrome in neonates with brachial plexus palsy has no prognostic value in predicting poor spontaneous motor recovery in patients with total-type brachial plexus palsy (190).
For nondiabetic mothers who deliver vaginally, neonatal BW 4400 g or greater was associated with a significant increase in the adverse neonatal outcomes of shoulder dystocia or brachial plexus injury, whereas neonatal BW 4800 g or greater was associated with a significant increase in the adverse maternal outcomes of postpartum hemorrhage or third- or fourth-degree perineal tears (11).
Prognosis. The prognosis and natural history of neonatal brachial plexus palsy depends on the extent of the initial injury. The pure forms of Erb-Duchenne palsy (ie, C5-C6) and pan-plexus palsy have a higher incidence of nerve avulsions than the extensive form of Erb palsy (ie, C5-C7) (175). Rapid and useful motor recovery is typical with Erb-Duchenne palsy and the upper root levels (C5 and C6) of pan-plexus palsy, in contrast to the poor prognosis of motor recovery with lesions of the lower root levels (C8 and T1) of pan-plexus palsy (168). Recovery of sensory function is much more frequent and occurs to a greater degree than recovery of motor function (168).
The prognosis and natural history depend, at least in some cases, on various circumstances of delivery (10). For example, spontaneous recovery of shoulder abduction and elbow flexion in newborns with Erb palsy is significantly worse among those with vaginal deliveries who were born breech compared with those born with cephalic presentations (61; 10). Obstetric brachial plexus palsy after a breech delivery is more typically the result of avulsion of the upper roots, an injury that cannot be treated satisfactorily by microsurgical grafting and carries a considerably worse prognosis for shoulder function (175; 61).
Determination of whether the injury is preganglionic or postganglionic through imaging and clinical exam can help predict the extent of motor recovery (72). Usually, preganglionic avulsion injuries are less likely to spontaneously recover motor function without surgical intervention. Injury to the phrenic, long thoracic, dorsal scapular, scapular, sympathetic chain, or the thoracodorsal nerve portends a poor recovery (72).
The Mallet Classification is a widely used tool that categorizes motor function of the shoulder to degrees of brachial plexus injury. The Mallet score looks at movement of the hand to mouth, neck, and spine and global abduction and external rotation. The lowest score given for no function is 1, and the score for normal function is 5. Summation of all these movement scores gives the overall Mallet score (133). In approximately 20% of cases, the Mallet score cannot be applied because of a discrepancy between the deficiency of shoulder abduction and shoulder external rotation (08). On this basis, Al-Qattand and El-Sayed concluded that “documenting the deficits in shoulder abduction and external rotation are best done separately and this can be accomplished by using other grading systems” (08). Narakas and colleagues also developed a classification of brachial plexus injury for infants aged 3 weeks and older for predicting the prognosis of spontaneous recovery depending on the severity of the brachial plexus injury, which is a strong predictor of outcome (128; 154; 57; 72). In the Narakas classification, poor recovery was less than half the normal range for elbow flexion and shoulder abduction (128). Narakas and colleagues found that Group I with Erb palsy (C5-6 injuries) had the best prognosis and occurred most commonly. Group II with C5-7 injuries had a poorer prognosis than Group I. Group III had involvement of C5-T1 and presented with a flail extremity, and Group IV with Horner syndrome in addition to C5-T1 involvement occurred in 4% of cases and had the worst prognosis.
When elbow flexion is considered in isolation, elbow flexion recovers spontaneously except in rare cases, although recovery occurs later in more severe injuries (77). On this basis, the authors considered it doubtful that nerve reconstruction could improve elbow flexion more than the likely spontaneous recovery in infants with obstetric brachial plexus injuries (77), although such procedures are increasingly being recommended (120; 124).
In a systematic review of brachial plexus palsy that included studies reported from 1966 to 2001, Pondaag and colleagues concluded that recovery occurs in approximately 70% to 80% of patients, with the remaining patients having residual deficits (138). Most patients with brachial plexus palsy diagnosed at birth recover from the neurologic deficit (06; 138). However, those who did not recover during the 3- to 6-month period require surgical intervention.
In a population-based study of 38,749 births during 1999 to 2001, Lagerkvist and colleagues reported that the incidence of brachial plexus palsy was 2.9 per 1000 live births (100). By 18 months, most infants had recovered with only 18% showing persistent brachial plexus palsy. At 3 months of age, the predictive value of regained elbow flexion, shoulder external rotation, and forearm supination for complete recovery was 100%, 99%, and 96%, respectively. Noetzel followed 80 patients with brachial plexus palsy who did not recover by 2 weeks of age and noted complete recovery was seen in 66% of patients by 6 months of age. Nine percent of patients demonstrated 3/5 strength in the triceps and biceps by 6 months and had residual weakness of 4/5 strength in triceps and biceps. Fourteen percent of subjects continued to have severe weakness in all muscle groups and were not antigravity by 6 months (122). Foad and colleagues performed an evidence-based review summarizing the data regarding prognosis using the Narakas classification and found that approximately 64% of group I and II have spontaneous recovery of biceps function at 3 months of age; this is consistent with conclusions from other studies that saw spontaneous recovery rates of approximately 66% (122; 80; 138; 57).
The decision to proceed with surgery for brachial plexus palsy is usually made by 6 months of life and is based on the clinical course as well as imaging findings suggestive of a poor prognosis for recovery. Depending on the severity of the injury and whether the distal basal lamina tubes remain intact, total recovery may occur in weeks or months (107). The distance between the proximal and distal stumps that the nerve axon must sprout determines the length of time for recovery. Spontaneous recovery is usually seen within the first 3 to 4 months after injury (107). By the age of 2 to 3 months, poor hand function is an absolute indication for surgical intervention (136; 107). Pondaag and colleagues also recommend surgery for patients who do not recover external rotation of the shoulder and elbow flexion or forearm supination by the age of 4 months (135). Clarke and Curtis recommended surgical exploration by 9 months if the patient is unable to place a cookie in the mouth with no more than 45 degrees of neck flexion, hence, a failed cookie test (128).
The specific surgical intervention depends on intraoperative electromyographic evaluations and visual observations of the brachial plexus. Surgical options for the patient are exploration and at times neurophysiologic testing in cases of neuroma-in-continuity with expectant management, neurolysis wherein the nerves are freed from inflammatory adhesions, neuroma excision and end-to-end anastomosis of the same nerve, and nerve grafting with local nerve by end-to-end anastomosis or remote nerves using sural nerve transplant or intrabrachial plexus transplant donor nerves (23; 65; 98).
Complications. Consequences of untreated neonatal brachial plexus injury may affect the glenohumeral joint of the shoulder and other joints of the arm as well as hand and finger function. The late sequelae include glenoid deformity or posterior dislocation of the glenohumeral joint (91), glenohumeral flexion contracture, and lost active shoulder extension (84). Neonatal brachial plexus injuries also result in structural changes in the affected limb bones, a finding found also in animal models, but these changes may be diminished if the microsurgical reinnervation is accomplished early enough (68). The most common deformities are limb length discrepancy, the development of contractures at the shoulder, elbow, and forearm as well as ulnar deviation of the wrist, and paralysis of the fingers (148; 70; 04). Zancolli and colleagues found that in 148 patients, the most common deformity was internal rotation contracture of the shoulder (72%) followed by supination contracture of the forearm (69%) and flexion contracture of the elbow (62%) (191). The amount of intraoperative correction is significantly associated with higher self-confidence and normal activities of daily living (73).
The photo exhibits a 25-year-old woman with obstetrical brachial plexus palsy sequelae and supination deformity of the forearm. (Source: Hamdi NB, Doubi M, Abalkhail TB, Mortada H. Clinical and psychosocial outcomes following c...
The photo exhibits an 8-year-old boy with obstetrical brachial plexus palsy sequelae and supination deformity of the forearm. (Source: Hamdi NB, Doubi M, Abalkhail TB, Mortada H. Clinical and psychosocial outcomes following cor...
Approximately two thirds of the children (69%) develop a glenohumeral abduction contracture; it is more common in those with upper neonatal brachial plexus injury (04).
Muscle denervation and degeneration are also complications of neonatal brachial plexus palsy. The most affected muscle is the subscapularis muscle, and its structural abnormality correlated with the degree of glenoid version (82). Abnormal rotator cuff muscles also correlated with posterior subluxation of the humeral head and the shape of the glenoid. The supraspinatus muscle differences correlated with the degree of superior subluxation of the humerus (82).
Neonatal brachial plexus has a negative influence on upper limb function and quality of life, and it has lifelong implications and impacts on a patient’s choices regarding education and profession as well as on work performance (177; 113).
Case 1 (unilateral Erb-Duchenne paralysis). A 4490 g male neonate was delivered via spontaneous vaginal delivery with no apparent complication. However, immediately after birth it was noticed that the baby did not spontaneously move his right arm. Initially his arm was flaccid, but over time it became clear that his distal function was good and proximally he was weak.
He presented to the clinic at 2 years of age for evaluation and possible treatment. He had worked with physical therapy, and the flexion in his arm had improved, but he still had considerable trouble elevating and externally rotating his arm. MRI showed right-sided pseudomeningoceles at the C5-C6 and C6-C7 lateral recesses that extended into the neural foramina with preservation of the right C6 and C7 nerve roots within the pseudomeningoceles. Spinal cord signal intensity and appearance remained normal.
Case 2 (bilateral Klumpke paralysis). JM presented to Boston Children’s Hospital at 7 months of age with the residua of bilateral Klumpke obstetric palsy (174). He was born on May 30, 1902, following a difficult labor. When the physician, JM Wells, arrived after 12 hours of labor, there was a face presentation with the chin posterior. Chloroform was given to complete relaxation, but the head could not be flexed. Application of forceps was tried, “but as there was absolutely no ‘give’ this was quickly discarded.” Several attempts were made at a version, and on the third attempt “the occiput engaged, and the labor proceeded normally, the right shoulder presenting at the pubes.” In the process, the attending physician noted that, “during one of the rests from the anesthetic, while I held my hand in the vagina with fingers against the chin using more or less pressure I heard and felt a decided click or snap. At first I thought the child’s neck was broken…” After delivery, the child was initially “narcotized by the chloroform but after slight artificial respiration came around all right.” When the child recovered from the anesthetic, the physician and the mother noticed that both arms hung limp from the shoulders without movement, whereas the head, neck, and legs moved normally. The child’s neck was examined, and no evidence of a fracture was identified.
He first moved his arms at the shoulders at 4 weeks. When he was examined on December 7, 1902 (approximately 6 months of age), his arms were abducted and internally rotated, the forearms flexed and pronated, the wrists somewhat extended, the fingers extended at the metacarpophalangeal joint and flexed distally, and the thumbs abducted to the plane of the hand. Passive extension at the elbow was “resisted with considerable force,” but the hands were flaccid. Voluntary motion of the upper extremities was limited to “elevation of the arms, and flexion of the forearms” (ie, the C5-6 myotomes). Movements of the head, neck, and legs were normal. Horner syndrome was not mentioned. The triceps reflex was absent bilaterally, but the knee jerks were normal. Pinprick sensation was present and judged normal in the upper extremities.
On February 4, 1903 (approximately 8 months of age), forearm flexion was “fair” (C5-6), the supinator muscles could be felt to contract (C6-7), the wrists could be slightly extended (C6-7), but deviated to the ulnar side, and slight movement had returned to the fingers of the left hand (except the middle finger) (probably C7-8 and not T1) and also the thumb and index finger of the right hand (probably C7-8 and not T1). Marked atrophy was noted in the forearm flexors (C7-8) and the intrinsic hand muscles (T1). The deltoids (C5), biceps (C5-6), and supinator (C6-7) muscles responded normally to electrical stimulation, whereas the triceps (C7-8) and all the muscles of the forearms (C7-8) and hands (T1) gave no response.
He learned to walk at about 1 year of age and had normal cognitive development. On the last reported examination in May 1905 (2 years of age), his gait was normal, but the paralysis of his arms had remained nearly the same, except that the grasp was somewhat stronger, especially on the left, though this was attributed to “recovery of the long flexor muscles, as the paralysis and wasting in the small muscles of the hand [was] still marked, and pronation of the forearms, flexion of the hands, and extension of the forearms [had] not improved, in spite of fairly regular treatment with massage and electricity.”
|
• The brachial plexus is formed by the C5-T1 nerve roots and consists of roots, trunks, divisions, cords, and branches. | |
|
• The five cervico-thoracic nerve roots merge to form an upper, middle, and lower trunk, and each trunk divides into anterior and posterior divisions, using the axillary artery as the anatomical landmark. | |
|
• The six divisions then form three cords: the posterior cord that contains posterior divisions of C5-T1, the lateral cord that contains the anterior divisions of the upper and middle trunks of C5-7, and the medial cord, which contains the anterior division of the lower trunk. | |
|
• The most important branches of the brachial plexus are the musculocutaneous nerve that is formed from the lateral cord, the median nerve combined from the lateral and medial cord, the ulnar nerve from the medial cord, and the radial and axillary nerves from the posterior cord. | |
|
• The upper brachial plexus, C5 and C6, innervates the deltoid, spinati, biceps, brachioradialis, biceps supinator, and flexor muscles of the forearm, whereas the lower brachial plexus innervates the intrinsic muscles of the hand. | |
|
• When examining a patient with a suspected brachial palsy, attention should be given to the position of the head, neck, and arm, noting concurrent nonmuscular torticollis, as well as fractures of the clavicle, humeri, and ribs. | |
|
• Obstetric brachial plexus palsy can result from excessive lateral traction and forceful deviation of the fetal head from the axial plane of the fetal body, particularly in association with shoulder dystocia, which increases the necessary applied peak tractional force to the nerve roots exiting the spine and also increases the time to deliver the fetal shoulders. | |
|
• The Seddon (1942) 4-category classification of the neuropathology of brachial plexus palsy involves these classes: Neurapraxia (Class I), Axonotmesis (Class II), Neurotmesis (Class III), and Root avulsion. Although complete recovery frequently occurs in brachial plexus palsy secondary to neurapraxia and axonotmesis, permanent loss of function occurs after root avulsion and neurotmesis if no surgical intervention is undertaken. Sunderland (1951) expanded this classification somewhat. | |
|
• Following nerve injury, the distal end undergoes a process called Wallerian degeneration where the myelin and damaged axon are broken down by the Schwann cells and macrophages and disappear. If the severity of the injury is too great, the neuron will undergo apoptosis or cell death; however, if the cell body remains intact, chromatolysis may reverse, and the axon may regenerate with the formation of a growth cone. |
The brachial plexus is formed by the C5-T1 nerve roots and consists of roots, trunks, divisions, cords, and branches. The five cervico-thoracic nerve roots merge to form an upper, middle, and lower trunk, and each trunk divides into anterior and posterior divisions, using the axillary artery as the anatomical landmark. The six divisions then form three cords: the posterior cord that contains posterior divisions of C5-T1, the lateral cord that contains the anterior divisions of the upper and middle trunks of C5-7, and the medial cord, which contains the anterior division of the lower trunk. The most important branches are the musculocutaneous nerve that is formed from the lateral cord, the median nerve combined from the lateral and medial cord, the ulnar nerve from the medial cord, and the radial and axillary nerves from the posterior cord. The upper brachial plexus, C5 and C6, innervates the deltoid, spinati, biceps, brachioradialis, biceps supinator, and flexor muscles of the forearm (83; 183). The lower brachial plexus innervates the intrinsic muscles of the hand (76).
When examining a patient with a suspected brachial palsy, attention should be given to the position of the head, neck, and arm. Concurrent nonmuscular torticollis may develop in association with brachial plexus injury, with the head turned away from the affected arm (94; 16; 79). If present, palpate the sternocleidomastoid to feel for a contractured muscle or a pseudotumor (128). Brachial plexus palsy and associated torticollis do not affect the clinical progression of the disease, nor does it have bearing on the severity of the palsy (79). In fact, 63% of patients recovered with conservative management of their torticollis (79).
Next, the neck and arms should be evaluated for fractures of the clavicle, humeri, and ribs because a so-called "pseudoparalysis" can be mistaken for a true brachial plexus injury. Pseudoparalysis occurs when the brachial plexus is indirectly compressed by bone fragment, local swelling, or involuntary arm splinting (128). Evaluation of shoulder function is also important because posterior dislocation of the shoulder has been associated with brachial plexus palsy (55; 166). Evaluation of the shoulder includes passive and active range of motion and holding the arm in 90 degrees of abduction and adduction as well as internal and external rotation of the joint (91). Also, one can palpate the pectoralis major, latissimus dorsi, and teres muscle to evaluate the contractile force (91).
Moreover, total brachial plexus palsy may also result in atony and flexed posture of the fingers (128). The presence of finger movement in the setting of brachial plexus injury may later result in the development of posterior subluxation or dislocation of the humerus head due to imbalance of the muscles during development of the infant’s shoulder (119). With total brachial plexus palsy the presence of a Horner syndrome generally conveys a worse prognosis for functional recovery (128; 53).
Asymmetry of the Moro reflex and tonic neck reflex also indicates brachial plexus injury (133). The Moro reflex disappears around 6 months in healthy infants; it is elicited by sudden extension of the neck that causes shoulder abduction and elbow and digit extension as well as finger spreading. The asymmetric tonic neck reflex is elicited by turning the head to one side, which causes extension of the upper and lower extremities on the side to which the head is turned and contralateral upper and lower extremity flexion. Also, one should test for sensation to light touch and pain with nail bed pressure and observing for aversive movements in the affected hand (133).
Brachial plexus palsy occurs as a result of stretch, tear, avulsion, or compression of the nerves. Obstetric brachial plexus palsy can result from excessive lateral traction and forceful deviation of the fetal head from the axial plane of the fetal body, particularly in association with shoulder dystocia, which increases the necessary applied peak tractional force to the nerve roots exiting the spine and also increases the time to deliver the fetal shoulders (56; 74; 76; 45). Direct compression of the fetal shoulder on the symphysis pubis may also cause an injury to the brachial plexus (45).
The neuropathology of brachial plexus palsy was originally described by Seddon (149), who classified nerve injury as:
Neurapraxia (Class I). Damage to the nerve sheath where there is a block of nerve conduction. The axon and nerve elements are left intact. The potential for regeneration is present. Neurapraxia is the most common form of brachial plexus injury.
Axonotmesis (Class II). Disruption of the axon of the nerve where the endoneurium is disrupted. However, the neural sheath (perineurium and epineurium) is left intact. The potential for regeneration is present.
Neurotmesis (Class III). Complete disruption of the postganglionic nerve (endoneurium, perineurium, and epineurium are transected) (149).
Root avulsion. Complete disruption of the ganglia from the spinal cord at both the anterior and posterior roots.
Although complete recovery frequently occurs in brachial plexus palsy secondary to neurapraxia and axonotmesis, permanent loss of function occurs after root avulsion and neurotmesis if no surgical intervention is undertaken.
Sunderland’s first and second degrees of peripheral nerve injury agree with Seddon’s Class I and II, respectively. However, in 1951 Sunderland expanded on Seddon’s classification of nerve injury in regard to whether transection of the nerve involves the epineurium and perineurium in the setting of damaged endoneurium (167). In Sunderland’s fourth degree injury, perineurium is damaged, and in the fifth-degree injury the nerve is completely transected with epineurium being damaged as well (167). Spontaneous recovery is not possible without surgical intervention with these two injuries (130).
Cell biology of neuronal sprout growth. When a peripheral nerve is injured or transected, the part of the axon that is still attached to the cell body is called the proximal stump, and the other segment is called the distal stump. Nerve injury prompts the recruitment of Schwann cells and glial cells to the area to remove debris. The distal end undergoes a process called Wallerian degeneration where the myelin and damaged axon are broken down by the Schwann cells and macrophages and disappear. Only the endoneurium remains. The cell body undergoes chromatolysis where the nucleus moves to the periphery, and the Nissl bodies or the endoplasmic reticulum is dispersed. The proximal end swells and undergoes some degeneration as well in a retrograde fashion. If the severity of the injury is too great, the neuron will undergo apoptosis or cell death. However, if the cell body remains intact, chromatolysis may reverse, and the axon may regenerate with the formation of a growth cone. Schwann cells that proliferate around the endoneurial tube or basal lamina tube in the distal stump form bands of Büngner, which help guide the sprouting axon for regeneration. Human axon growth rates can reach 2 mm/day in small nerves and 5 mm/day in large nerves (121).
|
• Obstetric brachial plexus palsy has an estimated incidence of 0.2 to 5 per 1000 live births. | |
|
• Spontaneous recovery rate is 60%, and some children suffer permanent impairment. | |
|
• Erb palsy, which involves the upper trunk (C5-C6), occurs in about 60% of brachial palsy injuries. An additional 20% to 30% of injuries are the more extensive form of Erb palsy involving C7, and 10% to 20% have total or pan-plexus injuries involving C5-T1. Klumpke palsy is rare. | |
|
• Suggested risk factors for obstetric brachial plexus injuries include shoulder dystocia, macrosomia (birth weight > 4 kg), maternal diabetes mellitus, small maternal stature, maternal obesity, excessive maternal weight gain in pregnancy, high maternal parity, prolonged pregnancy (postmaturity) or prematurity, prolonged second stage of labor, induction of labor, epidural anesthesia, secondary arrest of dilatation, persistent fetal malposition, instrument-assisted deliveries, downward traction of the fetal head, and vaginal breech extraction. | |
|
• Most cases of neonatal brachial plexus injuries have no known risk factors, and a significant proportion are now thought to occur in utero. | |
|
• Shoulder dystocia is defined as any birth that requires obstetric maneuvers to deliver the fetal shoulders, and it is the highest known risk factor for brachial plexus injury. |
Obstetric brachial plexus palsy has an estimated incidence of 0.2 to 5 per 1000 live births, and some studies report that the incidence in the United States is decreasing (165; 138; 14; 58; 45; 59; 180; 90; 125). It was previously believed that 80% to 95% of all injuries are mild and most neonates recover in the first 2 months; however, evidence shows that the spontaneous recovery rate is 60% and some children suffer permanent impairment (80; 138). Erb palsy, which involves the upper trunk (C5-C6), occurs in about 60% of brachial palsy injuries, making it the most common type of brachial plexus injury. An additional 20% to 30% of injuries are the more extensive form of Erb palsy involving C7, and 10% to 20% have total or pan-plexus injuries involving C5-T1. Klumpke palsy, which is an isolated lower root injury involving C8-T1, is a rare entity with conflicting data on its incidence (66).
Erb-Duchenne C5-C6 palsy, occasionally bilateral and complicated by phrenic nerve injury, is the most frequent form of obstetric brachial plexus palsy after a breech birth (175). The more extensive form of Erb-Duchenne palsy (ie, C5-C7, rather than C5-C6) and pan-plexus palsy (ie, C5-T1) are particularly frequent after vaginal delivery with complicated cephalic presentations (175).
Risk factors. Suggested risk factors for obstetric brachial plexus injuries include shoulder dystocia, macrosomia (birth weight > 4 kg), maternal diabetes mellitus, small maternal stature (ie, producing cephalopelvic disproportion), maternal obesity, excessive maternal weight gain in pregnancy, high maternal parity (ie, 6 or more), prolonged pregnancy (postmaturity) or prematurity, prolonged second stage of labor, induction of labor, epidural anesthesia, secondary arrest of dilatation, persistent fetal malposition, instrument-assisted deliveries (ie, vacuum extraction and forceps delivery), downward traction of the fetal head, vaginal breech extraction, and lower socioeconomic status (26; 27; 165; 112; 74; 78; 88; 114; 154; 14; 45; 57; 172; 126; 180; 90; 187; 12; 52; 75; 140). The strongest risk factors for obstetric brachial plexus palsy are shoulder dystocia, macrosomia (especially infant birthweight of 4400 gm or more), and vaginal breech delivery (114; 01; 54; 126; 02; 59; 11; 176; 52). Risk of obstetric brachial plexus palsy increases progressively with increasing fetal size, with a 2.5-fold increased risk for 4001 to 4500 g neonates and a 21.0-fold increased risk for neonates greater than 4500 g, compared with the risk for infants of normal size (ie, 2501-4000 g) (112; 114).
Risk factors for a permanent injury with obstetric brachial plexus palsy include high maternal body mass index, shoulder dystocia, fractured humerus, and fetal asphyxia (14; 52). Fracture of the clavicle in vaginal deliveries is significantly more frequent with transient brachial plexus injuries, possibly reflecting a protective effect (14). Because intrapartum peak forces applied by the clinician are significantly lower in routine deliveries than difficult deliveries, infants born following routine deliveries are more likely to develop Erb palsy and ultimately good recovery, whereas those born following difficult deliveries are more likely to develop total palsy and have poor functional recovery (54). Increasing gestational age and birthweight have a stronger effect on the risk for birth injury among cephalic vaginal deliveries than among vaginal breech deliveries (93).
Among 566 births with shoulder dystocia, brachial plexus injury was observed in 88 (16%), and permanent sequelae were detected in 12 (2%) (52). Maneuvers other than McRobert's (advanced maneuvers) were used more often, and clavicle fracture was seen more often in the group with plexus injury. Brachial plexus injury was observed 4.7 times more often in infants who were delivered with advanced maneuvers and 3.6 times more often in infants with clavicle fractures at birth.
In breech presentations, obstetrical brachial plexus palsy mainly results from “faulty performance of the manoeuvres that are needed to deliver the shoulders,” and there is a high frequency of root avulsions in breech deliveries of low birthweight infants (168; 27).
Shoulder dystocia. Shoulder dystocia, reported in 0.2% to 3.3% of all births, occurs due to the discrepancy between fetal shoulder size and the maternal pelvic inlet (62). The reported incidence of obstetric brachial plexus palsy after shoulder dystocia varies widely from 4% to 40% (45). Shoulder dystocia is anticipated to cause anterior shoulder involvement, which would produce a higher frequency of right obstetric brachial plexus palsies because the left occipito-anterior presentation is most common; nevertheless, posterior shoulder involvement is frequently seen (87).
Shoulder dystocia is defined by the American College of Obstetrics and Gynecology (ACOG) as any birth that requires obstetric maneuvers to deliver the fetal shoulders, and it is the highest known risk factor for brachial plexus injury (164; 58). Shoulder dystocia is often encountered unexpectedly--either when downward traction of the fetal head fails to deliver the shoulders, if there is extensive fetal vertex molding in prolonged labor, or if the fetus shows the “turtle sign” (19). Turtle sign refers to the retraction of the presenting chin into the maternal perineum due to bilateral shoulder dystocia. The most reliable predictor for shoulder dystocia is a previous episode of shoulder dystocia (43). Although shoulder dystocia is more common in macrosomic babies (ie, birthweight more than 4000 gm), fetal macrosomia is not a reliable predictor of shoulder dystocia (127).
Ultrasound examination is an unreliable mechanism in detecting fetal weight, with only 62% to 66% accuracy in detecting weight within 10% of the actual fetal weight (30).
ACOG recommends delivery via Cesarean section for babies weighing more than 5000 gm but does not have any current delivery recommendations for prevention of shoulder dystocia (39). For every 14 fetuses with an expected birth weight of more than 5000 gm delivered by cesarean section, one case of brachial plexus birth palsy can be prevented (40).
There are several maneuvers that can be implemented during vaginal delivery to relieve shoulder dystocia and, thus, prevent brachial plexus injury. The McRoberts maneuver refers to the positioning of flexed maternal thighs towards the maternal chest to slide the maternal pubic bone over the fetal anterior shoulder (89). This maneuver, coupled with suprapubic pressure, resolved 25% of cases of shoulder dystocia in one study (103). If the McRoberts maneuver fails to relieve the shoulder dystocia, rotational forces like the Woods’ corkscrew maneuver and Rubin maneuver can be applied. The Woods corkscrew maneuver applies force on the anterior surface of the posterior shoulder whereas the Rubin maneuver applies force on the posterior shoulder. The Rubin maneuver had a success rate of 66% and a birth injury rate of 14%. The Woods corkscrew maneuver had a success rate of 72% and birth injury rate of 9.5%. It is important to note that these maneuvers are usually performed after, or with, the McRoberts maneuver complicating the reporting of success and birth injury rates (81). The Zavanelli maneuver, or cephalic replacement, pushes the fetal head back into the mother so that the obstetrician can attempt a C-section and is rarely performed in the United States; consequently, there are very few reliable data in the literature to assess its rate of success or birth injury (103).
In a retrospective review of 46 children with neonatal brachial plexus palsy and shoulder dystocia, the incidence of brachial plexus palsy persistence was significantly higher at 2 years of age when more than three maneuvers were used or when the duration of the impacted shoulder lasted more than 120 seconds (44).
A strategy of prompt identification of shoulder dystocia accompanied by cessation of axial fetal head traction can decrease the risk of brachial plexus strain, injury, or tear, whereas performance of exact obstetrical maneuvers allowed delivery of fetal shoulders without permanent obstetrics brachial palsy or cerebral morbidity (71).
Closer attention to optimal management of shoulder dystocia has improved birth outcomes: in Sweden, obstetric brachial plexus palsy in vaginally delivered infants in a cephalic presentation at birth decreased during the period 1997–2019 despite an increase in important risk factors, including shoulder dystocia (115).
Mode of delivery. Brachial plexus palsy is the most common type of injury in vaginal breech delivery (93).
Although cesarean section is widely perceived as protective against obstetric brachial plexus injury, a systematic review identified 299 infants who sustained brachial plexus injury after cesarean section, half (53%) of whom had risk factors for likely challenging handling/manipulation of the fetus prior to delivery, in the presence of considerable maternal or fetal concerns or in the presence of poor access due to obesity or adhesions (85).
Cases with no known risk factors. Most cases of neonatal brachial plexus injuries have no known risk factors, and a significant proportion are now thought to occur in utero (96; 48; 87; 74; 63; 88; 14; 45; 57; 126). In a case in which the brachial plexus injury involved the posterior shoulder following a spontaneous delivery without forceps or manual rotation, with delivery effected using only the McRoberts maneuver, the authors hypothesized that maternal expulsive forces combined with lodging of the posterior shoulder on the sacral promontory caused the injury (74). Neonatal brachial plexus palsy can occur after cesarean section, sometimes in association with uterine pathology (eg, bicornuate uterus or uterine fibroids) (48; 63; 05; 126).
Transvaginal ultrasound showing a cross-section of a bicornuate uterus, with two cavities or "horns" visible at the left and right, respectively. In the "horn" to the right, a gestational sac is visible, with a diameter of 5.7 ...
In addition, electrophysiological studies have demonstrated evidence of denervation on the day of birth, which is not attributable to a birth-related injury (96). Possible mechanisms of intrauterine brachial plexus injury include the endogenous propulsive forces of labor, intrauterine maladaptation or failure of the shoulders to rotate, impaction of the posterior shoulder behind the sacral promontory, and uterine anomalies (eg, fibroids, an intrauterine septum, or a bicornuate uterus) (48; 74; 45). Indeed, fetal macrosomia is a risk factor for obstetric brachial plexus palsy regardless of whether the delivery is vaginal or by cesarean section (112).
Temporal trends. The epidemiology of obstetric brachial plexus palsy in the United States may be changing over time due to population-level changes in obstetric care, particularly a significant increase in the rate of cesarean delivery (38); indeed, the rate of obstetric brachial plexus palsy declined from 1.7 to 0.9 cases per 1000 live births in the interval from 1997 to 2012, in parallel with increasing rates of cesarean delivery. Cesarean section is associated with a decreased risk of obstetric brachial plexus palsy but does not eliminate the risk completely (48; 63; 114; 154). In particular, for singleton pregnancies with breech presentation or fetal macrosomia, the frequency of neonatal brachial plexus palsy can be reduced with planned cesarean delivery (112; 78). However, this is controversial because a policy of elective cesarean section for fetal macrosomia would require 148 to 258 cesarean sections to prevent a single persistent injury, and avoidance of operative vaginal delivery would require 50 to 99 cesarean sections per injury prevented (97). Indeed, a decision-analysis study to estimate the potential effectiveness and monetary costs of a policy of elective cesarean delivery for fetal macrosomia diagnosed by ultrasound concluded that for the 97% of pregnant women who are not diabetic, a policy of elective cesarean delivery for ultrasonographically diagnosed fetal macrosomia is “medically and economically unsound” (144). The best approach in pregnancies complicated by diabetes and fetal macrosomia is less clear (144).
The physical findings of brachial plexus palsy are unique, so it is difficult to mistake it for other diagnoses. However, these findings could be considered in the differential diagnosis of cerebral injury, cervical spine injury, trauma, and dislocation of the upper extremity as well as an inherited autosomal-dominant brachial plexopathy called hereditary neuralgic amyotrophy in affected families (101; 131; 76; 110; 83; 17; 109). Many of these have brachial plexus palsy as a finding in addition to other characteristics. Also, a case report of an arachnoid cyst that communicated with the dura of the C7 nerve root showed the patient presented with symptoms of obstetric-induced brachial plexus palsy. When the lesion was resected, the patient eventually recovered function (118).
|
• Neonatal brachial plexus palsies are typically diagnosed during physical examination. | |
|
• There are three main diagnostic modalities in working up brachial plexus palsies: plain radiographs, MRI, and CT myelography. Because most cases resolve spontaneously, these tests are usually performed after 3 months of age. | |
|
• EMG and nerve conduction studies are not routinely performed in the assessment of brachial palsy injuries because these tests provide limited predictive value for the presence of specific root damage. However, nerve conduction studies are used to monitor operative progress by establishing a baseline. |
Neonatal brachial plexus palsies are typically diagnosed during physical examination. A thorough neurologic examination involves assessing for the presence of the Moro reflex and the asymmetric tonic neck reflex. The diagnosis of brachial plexus palsy is supported by the absence of reflexes that induce elbow flexion, wrist extension, and digit extension. Additionally, the presence of Horner syndrome may indicate lower root injury and generally conveys a worse prognosis for functional recovery (53). The presence of crepitus, gross deformities, or lower extremity involvement may suggest alternative diagnoses like humeral or clavicular fractures and cerebral hypoxia.
There are three main diagnostic modalities in working up brachial plexus palsies: plain radiographs, MRI, and CT myelography. Because most cases resolve spontaneously, these tests are usually performed after 3 months of age. Plain radiographs of the cervical spine, shoulder, clavicle, elbow, and hand help rule out fractures, dislocations, subluxation, septic arthritis, dysplasia, and other abnormal anatomy (41; 03). CT myelography offers the best visualization of rootlets at each level of the spinal cord and is, therefore, optimal for its use for detecting pseudomeningoceles that are associated with nerve root avulsions (178). MRIs have the advantage of being noninvasive, don’t involve exposure to radiation, and can allow for visualization of the spinal cord and brachial plexus, but this modality is less sensitive than CT myelography in detecting nerve root avulsions (13; 186). A preliminary study suggests that 3-D proton-density MRI can evaluate spinal nerve roots in infants with suspected brachial plexopathy, without the need for radiation, contrast agents, or sedation; if confirmed, this may allow for earlier determination of the severity of injury based on serial clinical assessments (18). A systematic review concluded that MRI is the most sensitive and specific diagnostic modality for identifying preganglionic nerve injuries (eg, pseudomeningoceles and rootlet avulsion, the latter of which has the poorest prognosis in this patient population and often dictates the need for surgical intervention) (67).
Of note, EMG and nerve conduction studies are not routinely performed in the assessment of brachial palsy injuries because these tests provide limited predictive value for the presence of specific root damage. However, nerve conduction studies are used to monitor operative progress by establishing a baseline (151). A meta-analysis, however, noted the overall poor quality of available studies but, nevertheless, suggested that the most methodologically sound studies of the prognostic value of early electrodiagnosis in neonatal brachial plexus palsy support the use of electrodiagnosis, at standardized timeframes, as a key prognostic modality for complementing clinical judgment and neuroimaging (179); this conclusion was challenged, however, and at present the general utility of electrodiagnosis for neonatal brachial plexus palsies is unclear (141; 181).
|
• Neonatal brachial plexus injuries generally require multidisciplinary management. | |
|
• Early surgical referral may improve outcomes in patients unlikely to recover sufficiently with conservative management. Outcomes are better than the natural history of the condition in appropriately selected patients with surgical management. | |
|
• The main goal of the surgery in infants with Erb palsy is to restore shoulder and biceps muscle function. | |
|
• Although there are no randomized trials comparing surgical reconstruction versus conservative treatment in infants with obstetrical brachial plexus palsy, some authorities have proposed that nerve reconstruction is indicated “when the result of nerve surgery is assumedly better than the expected natural recovery, [and] spontaneous recovery is absent or severely delayed” (137). |
Neonatal brachial plexus injuries generally require multidisciplinary management (163; 49; 117). Many children with conservatively managed neonatal brachial plexus palsy have good long-term shoulder and elbow outcomes (117).
Surgery. Early surgical referral may improve outcomes in patients unlikely to recover sufficiently with conservative management (163). Outcomes are better than the natural history of the condition in appropriately selected patients with surgical management (163). In a study of 425 conservatively and 99 operatively managed children with neonatal brachial plexus palsy, operative patients had similar recovery of active range of motion when compared with nonoperative patients for shoulder external rotation, elbow extension, forearm supination, Narakas grade 1 to 2 injury, shoulder abduction, and forward flexion, even though operatively managed patients had more severe presenting injuries on average (116). New treatment paradigms and prediction algorithms may facilitate appropriate surgical case selection (163; 185; 190).
The main goal of the surgery in infants with Erb palsy is to restore shoulder and biceps muscle function. In palsy involving C7 nerve roots, reinnervation of the triceps is important. In global palsy, the primary focus is on hand reinnervation and grasp function, followed by elbow flexion, shoulder function, and finally, elbow, wrist, and finger extension (106; 108; 171). Even primary C5-8 brachial plexus reconstruction can provide restoration of elbow flexion and provide most affected patients a sensitive and functional hand, although secondary surgery to improve shoulder and wrist function is often necessary (105). For patients with complete neonatal brachial plexus palsy, sufficient recovery of hand function to perform bimanual activity tasks is possible and should be a priority in surgical treatment (156).
Primary nerve repair or nerve transfer procedures using microsurgery have now replaced muscle and tendon transfer as primary treatment modality, starting as early as 3 months of age but no later than 6 months of age. Distal nerve transfers have a significant advantage over primary intraplexal repair in early recovery of elbow flexion and shoulder abduction, but the outcomes become similar after 9 months (173). Secondary procedures 12 to 18 months after the primary treatment include tendon transfer and contracture release (37). Patients with chronic lesions who cannot undergo or have not responded to reconstruction undergo secondary reconstruction. These procedures consist of arthrodesis, muscle releases, neurovascular tissue/muscle or tendon transfers, or tenodesis.
For a patient with Erb palsy, a supraclavicular exposure is sufficient to expose the C5-C6 roots. An incision is made through the skin and platysma behind the sternocleidomastoid’s posterior border to the clavicle. Then dissection through the omohyoid is performed to expose the clavicle with division of the subclavius muscle and the periosteum of the clavicle (130). One then identifies the pectoral nerve branching off the anterior division of the upper trunk to preserve it. The upper trunk and spinal nerves that lie between the anterior and middle scalene muscles are exposed by reflecting aside the fat pad in the posterior triangle of the neck (133; 15). Care must be taken to identify the phrenic nerve (anteriorly located on the anterior scalene muscle) and the spinal accessory nerve, which may be aided with direct electrical stimulation (133; 130). Commonly, the trunks are surrounded by fibrotic tissue due to the initial injury (133). Exploration may disclose avulsed ganglia, neuroma in continuity, a ruptured brachial plexus, or a pseudomeningocele.
Although there are no randomized trials comparing surgical reconstruction versus conservative treatment in infants with obstetrical brachial plexus palsy, some authorities have proposed that nerve reconstruction is indicated “when the result of nerve surgery is assumedly better than the expected natural recovery, [and] spontaneous recovery is absent or severely delayed” (137). Nerve grafts are harvested from sensory nerves such as the sural nerve, the medial brachial nerves, and antebrachial cutaneous nerves (133). Other sources include parts of the plexus where regeneration probably won’t succeed, like the medial cord, ulnar nerve, the C7 spinal nerve, and the spinal accessory nerve; however, the presence of a pseudomeningocele precludes the use of the nerve for grafting (133; 123).
Neurotization utilizes nerve transfers to connect an uninjured neighbor nerve to the distal portion of an injured nerve, which is useful in avulsion injuries. Best candidate donor nerves are spinal accessory, intercostal, medial pectoral, thoracodorsal, long thoracic, and subscapular nerves; however, in infants, the efficacy is unknown for the use of the long thoracic, pectoral, thoracodorsal, and subscapularis nerves (107).
Examination of each root sample on the distal stump by a neuropathologist intraoperatively for major trunks or connections with doubtful quality may be helpful in guiding the surgeon in evaluating the quality of the proximal and distal stumps for grafting. The characteristics used to judge the quality of the root are the fascicular pattern (meaning the number and arrangement of the fascicles) and the presence of fibrosis in the peri- or epineurium, the presence of Büngner bands, and the level of remyelination and number of ganglion cells (15). A retrospective review of the outcomes of 96 patients who underwent either primary (less than 3 months of age) or secondary surgical intervention for neonatal brachial plexus palsy found that there were significant improvements in shoulder function. Reconstruction of both axillary and suprascapular nerves yielded improved outcomes of shoulder abduction and external rotation, whereas the rerouting of latissimus dorsi or teres major tendons and lengthening of the extra-articular tendons significantly improved global shoulder function (170).
Neurolysis. Neurolysis involves the release of the nerves from adhesions and inflammation. Some studies suggest that neurolysis is an inferior technique compared to resection of the neuroma and nerve grafting methods (98; 104). However, other studies suggest that neurolysis may be beneficial in cases that only involve the upper and middle trunks of the brachial plexus rather than the total plexus (35; 32; 50; 69). Chuang and colleagues advocate neurolysis should be done to determine the extent of scarring and the severity of the nerve lesion. Less severe lesions would require only neurolysis as treatment where significant scarring warrants resection of the neuroma and nerve grafting (33). Laurent and Lee proposed that neurolysis should not be used when intraoperative electrophysiological recordings show greater than 50% drop in the amplitude of the muscle action potential; rather, neuroma resection is indicated (102).
Resection of neuroma in continuity. Another surgical treatment is total resection of the neuroma in continuity with nerve graft interposition rather than neurolysis. One concern is that resection of a neuroma in continuity would diminish motor function as a result of a loss of nerve fibers that cross the neuroma; however, aggressive resection has not been found to result in significant motor loss (28). As stated earlier, some surgeons rely on electrodiagnostic recordings to guide their approach to the repair whereas others’ standard of care uses the resection of the neuroma with nerve grafting alone (66). Once resection of the neuroma has taken place, nerve grafts are used to bridge proximal and distal nerve stumps to guide growing axons using usually autologous sural nerve grafts (107).
Cable grafting. Cable grafting utilizes sutures or glue to join nerve strands in order to produce a graft with the same diameter as the recipient nerve. This technique has not been extensively used in obstetric brachial plexus palsy (145).
Nerve transfer. Nerve transfer procedures involve coapting a nerve from outside (extraplexal) or inside (intraplexal) of the brachial plexus to a denervated brachial plexus nerve (123). This procedure is becoming more commonly used and is advantageous because only one interface is used as compared to the nerve graft where one has to connect two stumps (72). ‘‘Terminal nerve transfers’’ refers to the complete transection of the terminal portion of a donor nerve whereas “end to side nerve transfers” utilizes fascicles of the donor nerve and preserves the terminal portion of the donor nerve (123). Common donor nerves include the spinal accessory, medial pectoral nerves, intercostal nerves, contralateral C7, hypoglossal, and ulnar nerve fascicles (123; 72; 107). Recipient nerves may include the terminal branches of the axillary, radial, median, and musculocutaneous nerve as well as the suprascapular nerve (123). In the past, nerve transfers were used to improve rotator cuff and bicep function, but now studies are looking at elbow flexion and hand function (72). Transfer of an ulnar fascicle to the biceps branch of the musculocutaneous nerve (Oberlin transfer) provides greater early recovery of forearm supination compared with nerve grafting, with equivalent elbow flexion recovery (29).
Muscle transfer. Free muscle transportation is useful to restore elbow flexion and motor function of the fingers and wrist to attempt to restore prehension or grasping (42; 182). Previously, donor muscles used for reconstruction were the latissimus dorsi, gracilis and rectus femoris muscles. However, the best donor muscle is the gracilis muscle because the others are not as successful for improvement of finger function (42; 152). Neurotization of the free muscle transfer includes the use the spinal accessory nerve to the suprascapular nerve and the third to sixth intercostal nerves to the musculocutaneous nerve or the median nerve (42; 33). Also, some studies have demonstrated successful use of the contralateral C7 nerve root to restore extensor digitorum communis function (31; 182).
Botulinum toxin: Botulinum toxin type A may be used off-label as an adjuvant to physical therapy and surgery in moderate to severe obstetric brachial plexus palsy (60); ultrasound-guided injection may increase effectiveness and reduce adverse effects (60).
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Douglas J Lanska MD MS MSPH
Dr. Lanska of the University of Wisconsin School of Medicine and Public Health and the Medical College of Wisconsin has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Epilepsy & Seizures
Jan. 20, 2025
Sleep Disorders
Jan. 18, 2025
Neuro-Oncology
Jan. 14, 2025
Neuro-Oncology
Jan. 14, 2025
Neuro-Oncology
Jan. 14, 2025
Neuro-Oncology
Jan. 14, 2025
Neuro-Oncology
Jan. 14, 2025
Developmental Malformations
Dec. 26, 2024