Neuro-Oncology
Choroid plexus tumors of childhood
Jan. 14, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
The septum pellucidum is a non-neural dual membrane structure originating from the medial parts of the embryonic cerebral hemispheres. Right and left leaves of the septum are, therefore, part of the embryonic origin of the cerebral hemispheres. The opposing leaves are separated by a cavity in fetal life, which gradually becomes thinner and obliterates. Its posterior extension is the cavum Vergae. The roof is formed by the corpus callosum and the hippocampal commissure, and the posterior and inferior of the septum is bordered by the fornices. The midline cavities of the brain are often involved in malformations that affect the midline structures of the brain, such as callosal agenesis. Delay of the normal closure of the cavum septum pellucidum may be a first warning sign in routine ultrasound studies of the fetal brain. In this way, abnormalities of the cavities, mostly by size, may indicate the need for further examinations. The size of the cavum septum pellucidum after birth varies considerably. Normal variability versus a possible relationship to acquired brain disorders has caused a stream of studies, also discussed in this article.
|
• The cavum of the septum pellucidum is bordered by two leaflets that closely approximate during the first year of life. | |
|
• The cavum Vergae is a posterior extension of the former. | |
|
• The leaves of the cavum contain no vital structures. | |
|
• Pathologies of the cavum, as detected by MRI, include its persistence, as well as complete absence of the septal leaflets resulting in a single cavity. Both anomalies may form part of complex congenital disorders. | |
|
• Pathology of the cavum is not harmful in itself but may draw attention to pathology in adjacent neural structures. | |
|
• Increased width of the cavum is nonspecific but may reflect spatial compensation for lack of brain growth in the fetus or brain atrophy in adults. |
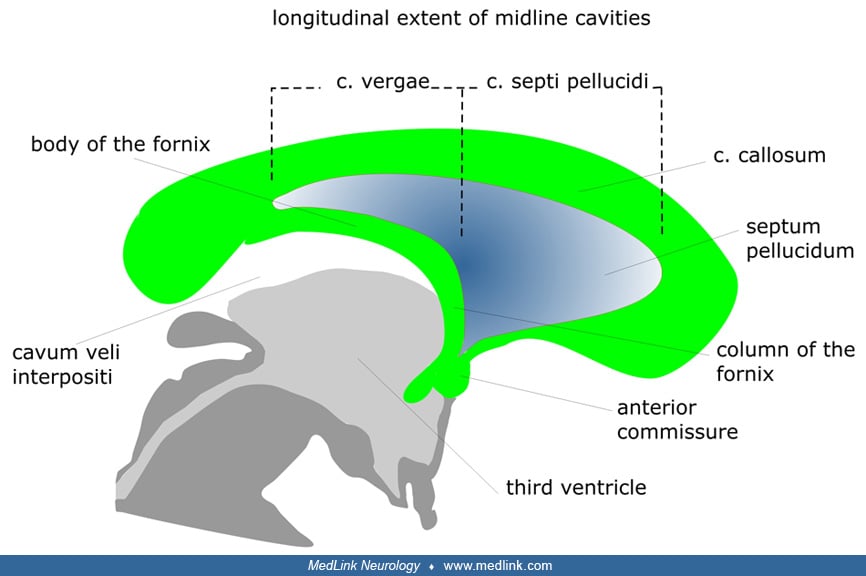
The septum pellucidum is a double vertical membrane that separates the corpus callosum from the columns of the fornix and intervenes between the lateral ventricles. The septum has right and left leaves, each of which is part of the respective medial hemispheric border. The anatomist Sylvius of Leyden University first described cavum septi pellucidi in 1671 (07). Cavum Vergae is a posterior extension of the cavum septi pellucidi, communicating with the cavum septi pellucidi but lying posterior to the columns of the fornix (70). In the early literature, these cavities were considered to be the fifth and sixth cerebral ventricles, respectively. They are not actually ventricles because they are not primarily part of the ventricular system, are not lined by cells of the ependyma, and do not contain choroid plexus. The anatomic boundaries of the cavum septi are the medial hemisphere walls on the lateral sides; the roof is formed by the corpus callosum. The cavum septi pellucidi is bordered posteriorly by the column of the fornix. The cavum Vergae is bordered anteriorly by the posterior border of the cavum septi pellucidi, inferiorly by the body of the fornix, and superiorly and posteriorly by the corpus callosum. Anatomically, the two cavities are not separated. Another cavity, known as the cavum veli interpositi, is part of the leptomeningeal space and intervenes between the roof of the third ventricle and the body of the fornices. When the corpus callosum is absent, the cavum septi becomes unroofed and, therefore open to the leptomeningeal space.
The formation of the cavities was detailed by Rakic and Yakovlev, who analyzed the brains of 113 fetuses and numerous vertebrate species. The human samples covered the crucial period of 13 to 14 weeks during which commissuration takes place (52). According to this study, the cavum septi is a part of the leptomeningeal space sealed off by the developing corpus callosum. The septum pellucidum is made of two opposed sheaths of tissue derived from the medial walls of the hemispheres. Its lower edge is bordered by the columns of the fornix (53). The inferior and posterior border of the septum pellucidum is formed by the columns of the fornix, which are part of the limbic system, connecting to the hippocampi. Because of their close anatomic relationship, absence of the septum leads to ectopia of the fornices and absence of the forniceal commissure. The lateral, ventricular surface of the septum pellucidum is covered with ependyma; the medial surfaces (when not fused) are poorly organized and appear glial in neonates. The cores of the pellucidal leaves contain small myelinated fibers (53). Dandy first described cysts of the cavities in 1931 (10).
The midline cavities are essentially temporary embryonic structures that involute during late pregnancy and infancy. Persistence of these structures beyond this period does not cause any symptoms but is statistically related to malformations and psychiatric disturbances, mainly dependent on size (Table 1).
The size of persistent midline cavities is differently measured because size may be measured by antero-posterior extent or by width. The former approach is generally used in MR studies of neuropsychiatric populations, eg, with schizophrenia (47). The latter approach is usual in younger groups where persistence of the structure itself is rated less significant than increased transverse size. It should be stressed that progressive decrease in width of the cavities during pregnancy and infancy parallels transverse growth of the cerebral hemispheres, and, in this regard, decrease of the cavities may be seen as compensatory to the increase of brain size. A significant correlation has been found between biparietal diameter and size of the cavum septi pellucidi (26).
|
Measurement by US or MRI in controls |
Size |
References | |
|
36 to 40 weeks fetal age |
Width |
<9,5 mm |
(40) |
|
Newborn 39 to 40 weeks of age |
Average width |
6.3 mm +/- 0.83 (1 sd) |
(26) |
|
Children and adults |
Maximal length |
< 6 mm |
(45) |
Persistent and enlarged midline cavities after birth. The cava septi pellucidi and Vergae are seen as part of normal development in the fetus and neonate. Persistence of these structures is common throughout infancy. Typically, at 6 months gestation, the posterior half of the fusion is complete. The anterior half does not fuse until after birth, making the incidence of cavum septi pellucidi in premature infants 100% (33). Generally, by 6 months of age, the process is complete (42), but the fusion is frequently not 100%, as there is often a small cavity near the genu of the corpus callosum (60).
The reported incidence of cavum septi pellucidi in normal adults varies enormously from 0.10% to 85% (47). Tsutsumi and colleagues applied MRI with the CISS sequence, a gradient-echo, in adults to obtain a better sensitivity for the interface between tissue and fluid in the cavities (69). Using the CISS sequence cavum septi pellucidi, cavum Vergae, and cavum veli interpositi were visible in unexpectedly high proportions: 67% in coronal sections and 91% in sagittal sections.
Earlier MRI studies indicated that the incidence of small cavum septi pellucidi (less than 5 mm in anterior to posterior length as seen on contiguous coronal MRI slices) is common (59% to 85%) in the normal healthy population (47; 32; 21). This suggests that small cavum septi pellucidi should be considered a normal variant of anatomy. However, enlargement of the cavum septi pellucidi (greater than 5 mm in length) was seen uncommonly in the healthy population (1% to 2.4%) and linked to developmental abnormality. Born and colleagues, using the evaluation method of Nopoulos and colleagues, studied three healthy groups of subjects: children, young adults, and elderly adults (47; 05). Cavum septi pellucidi was detected in 80% of the cases in the pediatric group, in 68% of young adults, and in 72% of the elderly adults. A cavum Vergae was noted in 22% of the children, in 39% of the young adults, and in 36% of the elderly subjects. There was no significant difference between the age-related groups.
Association with CNS malformations. The formation of the septum and the fusion of the septal leaflets are intimately related to the development of other midline structures such as the corpus callosum and medial temporal structures such as the hippocampus. Dysgenesis of the corpus callosum or the limbic system may be signaled by anomalies of the midline cava and septum on fetal ultrasound.
A wide range of cerebral malformations, especially those affecting the cerebral cortex, can be associated with an enlarged cavum septi. This association may be seen together with chromosome abnormalities, eg, 22q11 deletion (59; 04; 57; 09). In a large study of 260 fetuses, the linear correlation between the cavum septum pellucidum and biparietal diameter was noted (29). In this study, 37 fetuses with 22q11 deletion syndrome were included, and the cavum septi pellucidi was enlarged, with a mean Z score of 2.64 (p< 0.0001). Fetuses with a gestation of more than 22 weeks and a biparietal diameter of more than 50 mm had a dilated cavum septi pellucidi in 85.7% cases. A dilated cavum septi pellucidi may be an important sonographic marker for the presence of 22q11 deletion syndrome in association with conotruncal malformation and thymic hypoplasia (09). A retrospective cohort study by Gaiser and colleagues supported the above finding that an enlarged cavum septi pellucidi and hypoplastic and absent thymus can be used as a marker for 22q11.2 deletion syndrome (20).
A hallmark of all forms of holoprosencephaly is the absence of the cavum septum pellucidum, and attention to this structure is vital to ensure detection of the milder forms (24).
An association between congenital malformation syndromes and inborn errors that affect the fetal shaping process, ie, peroxisomal enzyme deficiencies, was also seen.
Association with craniofacial disorders. In Apert syndrome of acrocephalosyndactyly, an abnormal septum pellucidum is a regular feature. According to several studies, 23% of patients with Apert syndrome had abnormalities of the corpus callosum, and 17% had absent septum pellucidum (54; 67). A study of adult males with nonsyndromic cleft lip and palate showed a significantly higher incidence of enlarged cavum septi pellucidi; the incidence was calculated to be 8% in comparison to healthy controls (44). This association was mostly associated with cognitive deficits.
Association with congenital syndromes due to teratogen exposure. Studies have shown that midline CNS structures are developmental fields that are particularly susceptible to the teratogenic effects of alcohol. Enlarged cavum septi pellucidi is frequently seen in fetal alcohol syndrome (25). In an MRI series of 10 subjects with fetal alcohol syndrome, 50% had either an enlarged cavum septi pellucidi, cavum Vergae, or both (65). Additionally, studies by Swayze and colleagues showed that more severe facial dysmorphism is associated with midline brain anomalies, including corpus collosum abnormalities and cavum septum defects, in addition to ventricular enlargement and microcephaly (65). In utero exposure to valproate has been associated with midline brain abnormalities, typically absence of the septum pellucidum (35; 38).
Association with schizophrenia. Eight of 11 MRI studies until 2001 found increased prevalence of cavum septi pellucidi in patients with schizophrenia as compared to normal controls (11; 12; 13; 58; 62; 47; 32; 50). The remaining three studies showed no increased prevalence of enlarged cavum septi pellucidi in schizophrenia (27; 19; 21). In the study of Nopoulos and colleagues, the incidence of small-sized cava was comparable between patients and controls (47). However, the patient group had significantly higher incidence of large cavum septi pellucidi (ie, over 5 mm in length: 20.7% in patients vs. 3% in controls). The patients with large cavum septi pellucidi were all male. In addition, a study done on subjects with childhood-onset schizophrenia found that the incidence of enlarged cavum septi pellucidi was similar to those seen in patients with the adult onset of the disorder. However, the severity of the anomaly was worse in the childhood-onset sample; on average, the size of the cavum was much larger than those seen in the adult-onset group (45). Nopoulos and colleagues have reported significant inverse correlations between the actual size of cavum septi pellucidi and IQ scores, indicating the larger the cavum septi pellucidi, the lower the IQ. These two studies were done in subjects with schizophrenia (46) and subjects with nonsyndromic clefts of the lip and palate (44). A meta-analysis by Liu and colleagues addressed the large number of studies whose results hover on the threshold of significance (36). Ten cross-sectional and three longitudinal studies on the incidence of abnormalities of the cavum septum pellucidum in patients presenting with first episode schizophrenia were selected, all studies meeting standard criteria for epidemiological studies. The meta-analysis uncovered no significant differences between patients and healthy controls as an overall result.
Raine and colleagues studied 75 patients and demonstrated the association between the cavum septum pellucidum and a spectrum of antisocial behaviors (51). This finding appears to provide evidence of a neurodevelopmental brain abnormality in antisocial individuals and supports the hypothesis that early maldevelopment of limbic and septal structures predisposes to antisocial behavior.
Association with chronic traumatic encephalopathy (CTE). Chronic traumatic encephalopathy was formerly known as "punch drunk" syndrome, or dementia pugilistica, which refers to cognitive changes seen in boxers. The syndrome is not exclusively related to boxers but may present in all sports with liability to repeated head trauma.
An exhaustive literature review by Smith and colleagues gives credence to the presumed relationship between enlarged cavum septi and chronic traumatic encephalopathy (63). Two mechanisms are proposed: (1) general cerebral atrophy leading to compensatory widening of the cavum septi and (2) ventricular dilation and septal changes as a consequence of repeated transient increases in intracranial pressure. A study by Koerte and associates addressed differences between retired professional American football players and a control group of retired athletes without a history of repeated head trauma (“noncontact sports”) (31). The study involved comparison of 3T MRI images of the septal region in both groups. A significant increase of caval width was found in the first group. Both groups also differed substantially on cognitive testing, with the first group performing abnormally. A logical conclusion might be to relate increased size of the cavum to general cerebral atrophy.
In a large cohort study of 476 patients with repetitive brain injuries, data showed a significant association between the presence of cavum septum pellucidi or Vergae and decreased cognition in patients with decreased brain volumes (34). Long-term follow up on this cohort using the same standardized scales will provide more information.
Increased size of cavum septi pellucidi on fetal ultrasound. Increased use of ultrasound in pregnancy and its steady refinement in the screening for fetal disorders has put isolated increase of cavum septi in focus and prompted the question of whether it should be given prominence in the search for broader underlying disorders. Normative data on the size of the cava in normal fetuses during the second and third trimesters are provided by Tao and colleagues (68). Abele and colleagues retrospectively analyzed the width of septal cava between 18 and 40 weeks in a cohort in which chromosome analysis was done, resulting in 267 euploid and 139 aneuploid cases (01). In 42% of the fetuses with trisomy 21, cavum septi pellucidi was above the 95th centile. Findings in trisomy 18 and 13 showed the same trend. The authors concluded that the finding of an enlarged cavum septi in the second and third trimesters forms an indication for a search for chromosomal abnormalities. Interestingly, the study also provided evidence that the width of the cavum is linked to the biparietal diameter. Chaoui and colleagues confirmed the increased incidence in fetuses with chromosome 22q11 microdeletion (09).
Association of longitudinal shortening of cavum septum pellucidum with partial agenesis of the corpus callosum during the fetal stage. Shortening of the cavum on midsagittal ultrasound was found to be associated with partial agenesis of the corpus callosum in fetal measurements and useful in fetal diagnosis of partial callosal agenesis (29).
Absence of detectable cavum septum pellucidum. Prenatal sonography may fail to detect the cavum as the first warning sign of a cerebral malformation. Intrauterine hydrocephalus may destroy the septal lamina, or its presence may be masked by an interhemispheric cyst, which is often seen in association with callosal agenesis. Absence of the cavum may also be a presenting sign of holoprosencephaly (64) or septo-optic dysplasia (48). Prolonged follow-up of individuals presenting with apparently isolated absence of the cavum septum pellucidum during pregnancy is necessary, including MRI.
Space-occupying lesions associated with cavum septi pellucidi. Hemorrhage into the cavum has been reported in preterm infants with coexisting intraventricular hemorrhage (08) and in adults secondary to trauma and hypertension (28). Tumors of the cavum can develop (18). Large cava often occur in the brains of children or adults with generalized cerebral atrophy from any cause.
Other space occupying lesions involving the cavum septi are empyema associated with purulent meningitis (30; 49).
Recurrence of a previously closed cavum septi has been reported following the placement of an Ommaya reservoir for administration of chemotherapeutic with the tip against the septum (61).
Absence of the septum pellucidum. Prenatal sonography may fail to detect the cavum as the first warning sign of a cerebral malformation. Absent septum pellucidum can be diagnosed prenatally in the second trimester, but many cases are missed due to limitations, including obesity, uterine fibroids, polyhydramnios, or fetal presentations. A focused intermediate ultrasound at 24 weeks must be done to complete the screening. Following a positive screen, genetic counseling, karyotyping, and amniocentesis must be recommended, but families should be advised that up to 20% of septo-optic dysplasia diagnoses are made only in the neonatal period.
Intrauterine hydrocephalus may destroy the septal lamina, or its presence may be masked by an interhemispheric cyst, which is often seen in association with callosal agenesis. Absence of the cavum may also be a presenting sign of holoprosencephaly (64). The following categories are known to be associated with absence of the septum pellucidum: Apert syndrome, septo-optic dysplasia, holoprosencephaly, schizencephaly, rhombencephalosynapsis, and fetal alcohol syndrome. The association of congenital absence of the septum pellucidum, optic nerve hypoplasia, and often pituitary insufficiency is known as "septo-optic dysplasia," a midline cerebral dysgenesis (14; 56).
Holoprosencephalic brains lack a septum pellucidum, and this may serve as a marker for the diagnosis on prenatal ultrasound investigation of the fetal brain. The absence of a septum pellucidum has also been described as part of a syndrome of bilateral full-thickness porencephaly, ie, open-lip schizencephaly and neuronal migration disturbance (02). Absence of the septum is also seen in closed-lip schizencephaly (37).
Absence of the septum, in most cases associated with fusion of the fornices, is also seen in association with rhombencephalosynapsis (03). The fornices are normally suspended from the inferior edge of the septum. As a result of the absence of the septum, the fornices become displaced or interrupted. As the fornices form part of the limbic system, their complete absence may be expected to cause severe deficiencies. In a group study of patients with septo-optic dysplasia, hippocampal abnormalities were present in a significant proportion and related statistically to the degree of mental deficiency (55). Nagaraj and colleagues offered a useful binary flowchart for the differential diagnosis of absent cavum septum pellucidum, which stepwise, helps to identify holoprosencephaly spectrum, callosal anomalies, and optic nerve hypoplasia (41).
Prenatal diagnosis of septal abnormalities. Neuroimaging of intracranial structures using transabdominal ultrasonography has gained significant technological advances. As one report suggests, the cavum septi pellucidi is reliably visible and its size can accurately be quantified. In normal fetuses the cavum septi pellucidi should always be visualized between 18 and 37 weeks with a biparietal diameter of 44 to 88 mm. Failure to observe the cavum septi pellucidi in this interval, or possibly the presence of a large cavum septi pellucidi, may indicate abnormal cerebral development and demands further investigation by fetal MRI. In this way, the finding of an absent septum pellucidum may lead to the diagnosis of the causative malformations (23). An enlarged cavum septum pellucidum observed on fetal ultrasound during the second trimester was found to be associated with congenital abnormalities (22). Conversely, absence of the cavum septi pellucidi prior to 18 weeks, or later than 37 weeks, is a normal finding (17). In a follow-up study of premature infants, it was found that the time of disappearance of the cavum septi had no relationship with developmental parameters (43).
Fetal life visualization of cavum septi pellucidi between 18 and 20 weeks of gestation implies normal brain development. Visualization of septi pellucidi is mandatory on anomaly scan. The absence of cavum septi pellucidi in the second trimester, by itself, is not a marker of severe malformation. Associated abnormalities, including septo-optic dysplasia, holoprosencephaly, agenesis of the corpus callosum, schizencephaly, Chiari II malformation, and other migration disorders, need to be considered (72).
The cavum septi pellucidi is usually diagnostic incidentally, and it is typically asymptomatic. Persistent cavum septi pellucidi is identified in approximately 20% of normal subjects. An elevated presence of the cavum septum pellucidum is reported in several psychiatric conditions, including bipolar disorder and schizophrenia, whereas the widely separated cavum leaflets of more than 1 cm are associated with disturbed brain development. It is important to understand that the cavum septi pellucidi, by itself, is harmless, and outcome depends on associated anomalies.
Although rare, cysts of the cavum septum pellucidum can cause significant neurologic dysfunction. Cysts of the cavum septum pellucidum can be classified as communicating and noncommunicating. Secondary communicating cysts can be formed due to trauma, spontaneous rupture, or surgery. Headache is the most common consistent presentation due to intermittent hydrocephalus and is usually provoked by positional changes and maneuvers that cause an increase in intracranial pressure. Treatment is indicated when the patient has clinical signs of hydrocephalus as well as imaging evidence of the cavum septi pellucidi cyst, direct compression of the adjacent tissue by the cyst, and mental status changes or focal neurologic deficits from the cyst (06).
Treatment options include open surgical intervention, conventional shunting, stereotactic fenestrations, and several endoscopic interventions. Surgical intervention usually carries a good prognosis, with resolution of symptoms.
A 17-year-old male presented for psychiatric evaluation after developing psychotic symptoms of hallucinations and delusions 4 weeks prior. He was the product of full-term gestation with no complications, with the exception of maternal smoking. According to his mother, the boy met all developmental milestones “within normal limits,” but notably later than his siblings. He was also much more socially isolative and immature compared with his siblings. He did poorly in school and was held back in the first grade due to academic and social nonprogression.
On mental exam he was poorly groomed and had poor eye contact. His thoughts were disorganized, and he admitted to ongoing auditory hallucinations and persecutory delusions. On physical exam he exhibited some minor physical anomalies such as high-steepled palate and curved fifth finger. He also demonstrated some neurologic “soft signs” such as impersistence of lateral gaze and persistence of a developmental reflex (palmomental reflex).
Neuropsychologic testing indicated a full-scale IQ of 77 (borderline intellect range). MRI scan showed a combined cavum septi pellucidi and cavum Vergae, indicating complete lack of fusion of the septal leaflets during development.
The patient was diagnosed as having schizophreniform disorder. He was treated with antipsychotic medications and his psychosis improved but persisted. After 6 months his diagnosis was changed to schizophrenia, undifferentiated subtype.
The septum pellucidum starts developing at 10 to 12 weeks of intrauterine life from the commissural plate or primitive lamina terminalis. The development is completed around 17 weeks of age and is closely associated with the development of midline structures.
Development of the septum pellucidum is intimately connected with development of the corpus callosum. According to the classic study of Rakic and Yakovlev, the cavum septi forms part of a section of the interhemispheric leptomeningeal space, which is sealed off by the developing corpus callosum (52). This view, now generally accepted, holds that the corpus callosum develops extracerebrally. Raybaud provides an excellent review and summary of the work of these authors (53). At the time of the outgrowth of the telencephalic hemispheres from the rostral end of the prosencephalon, the anterior midline ridge connecting the developing telencephalic outgrowths is called the lamina reuniens. The hippocampal and anterior callosal commissures and the hippocampal fornices develop within this ridge. The study by Rakic and Yakovlev ended a longstanding dispute on the mode of origin of the corpus callosum (52). They observed that the embryonic corpus callosum develops within a separate, phylogenetically new structure, which they named the glial sling. This structure is a glial ridge that develops from the medial parts of the hemispheres as a separate outgrowth, dorsal and anterior to but not forming part of the lamina reuniens. Fusion of these ridges across the midline creates the glial sling that bridges the interhemispheric meningeal space, creating the bed for the future corpus callosum. In this way, a closed space is created in the gap between the corpus callosum and the structures developing from the lamina reuniens. This is the cavum septum pellucidum. It follows from this reasoning that the cavum septum pellucidum is an extracerebral space. The lateral leaves of the cavum septum pellucidum are formed by the medial hemispheric walls, which fuse later in development.
In the normal development of the cava and in cysts of the cava, this space is not in communication with the ventricular system. Interestingly, cavum septi develops as a transient structure during fetal life, which disappears gradually by approximation of its lateral leaves, synchronous with the growth of the frontal lobes. Its persistence is seen in widely different prenatal-onset brain diseases, including acquired fetal disorders. Consequentially, it may be assumed that impaired transverse growth of the brain at the level of frontal lobes causes persistence of the cavum septi irrespective of the nature of its cause (genetic vs. acquired). Sometimes this relative redundancy of space causes enlargement of the interhemispheric distance.
The leaves of the cavum septum pellucidum normally start to fuse at 34 weeks' gestation. Thirty-six percent to 50% of term babies have cavum septi pellucidi by CT and ultrasound (42), whereas up to 85% have cavum septi pellucidi by autopsy studies (07). Ten percent have cavum septi pellucidi at 1 year by most imaging and pathological reports. In adulthood, incidence usually ranges from 3% to 20% (07).
Cavum Vergae is seen in all 6-month fetuses but in only 30% of term infants by postmortem studies (07). Cavum Vergae usually accompanies cavum septi pellucidi, with an incidence in adults of less than 2%. Cavum Vergae without cavum septi pellucidi has also been reported (07; 39).
Cavum septi is a harmless condition in itself. It forms part of a large and divergent group of disorders with embryo-fetal onset. Prevention should be part of the approach to the respective causal disorders.
The cavum septi pellucidi has been confused with the third ventricle and the corpus callosum on ultrasound. The distinction is evident on CT, MRI, and postmortem analysis. The differential diagnosis of cavum septi pellucidi includes velum interpositum cyst, ependymal cyst, ventricular loculation, vein of Galen aneurysm, dilated third ventricle, and neuroepithelial cysts.
Cavum veli interpositi is a triangular-shaped cavity that extends below the splenium of the corpus callosum and the column of fornix and above the internal cerebral veins, with the apex of the triangle reaching anteriorly as far forward towards the foramen of Munro.
A cyst of the cava may be differentiated from persistence of the cava by the lateral convexity of the septal leaves, scalloping of the inferior corpus callosum, and mass effect on other adjacent structures. Vein of Galen aneurysm is distinguished from cavum septi pellucidi using color doppler. A dilated third ventricle is distinguished by its location between thalami (23).
An enlarged cavum septum pellucidum, more than 1 cm, or its presence beyond infancy is considered pathological and should warrant further diagnostic workup. Diagnostic workup also depends on the clinical context. There are no published data on whether practitioners should vary their approach for the fetal versus the postnatal period. However, according to most experienced practitioners, the approach in both periods is similar.
An enlarged cavum septum pellucidum is mostly associated with hydrocephalus, growth restriction, and chromosomal translocation, so fetal karyotyping must be done.
In some cases, cysts of cavum septi pellucidi or cavum Vergae may compress the cerebral aqueduct or the foramina of Monro, resulting in hydrocephalus. Patients eventually develop bifrontal or occipital headaches. Gait abnormalities and change in mental status follows. MRI is required for further characterization in these patients. Specialized techniques to analyze the flow of cerebrospinal fluid through the foramen of Monro, third ventricle, and cerebral aqueduct may be useful in selected patients (72).
Treatment indications for cavum septum pellucidum include direct compression of the surrounding tissues by the enlarging cyst, clinical signs and symptoms of hydrocephalus, and radiological evidence of the cyst with mental status changes or focal deficits attributed to the cyst. The goal of treatment includes relieving the pressure caused by mass effect. Treatment options include open surgical or endoscopic methods. Three endoscopic approaches have been described: (1) frontal approach on the coronal suture 3 cm from the midline structure, targeting the lateral ventricle on its frontal horn; (2) frontal approach, including puncturing the cyst and fenestration of the walls of the cyst; (3) an occipital method in which a burr hole is made to optimize the trajectory into the atrium of the lateral ventricle, which allows both of the leaflets to be reached perpendicularly (16).
Neuroendoscopic procedure is considered the treatment of choice for symptomatic cavum septum pellucidi. Results of endoscopic procedure alone have shown complete resolution of symptoms, thereby avoiding the use of implantable cerebrofluid shunt (15; 71).
Asymptomatic septal cysts represent no risk to pregnancy.
Asymptomatic septal cysts represent no risk for anesthesia.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.
Kapil Arya MD
Dr. Arya of Arkansas Children's Hospital/UAMS has no relevant financial relationships to disclose.
See ProfilePraveen K Ramani MD
Dr. Ramani of University of Arkansas for Medical Sciences has no relevant financial relationships to disclose.
See Profile
Ganeshwaran H Mochida MD
Dr. Mochida of Boston Children's Hospital and Harvard Medical School has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Neuro-Oncology
Jan. 14, 2025
Neuromuscular Disorders
Dec. 29, 2024
Developmental Malformations
Dec. 26, 2024
Developmental Malformations
Dec. 26, 2024
General Child Neurology
Dec. 26, 2024
Developmental Malformations
Dec. 14, 2024
Developmental Malformations
Dec. 12, 2024
Developmental Malformations
Nov. 22, 2024