General Neurology
Use of focused ultrasound in neurologic disorders
Jan. 13, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Cervical spondylotic myelopathy is a progressive noninflammatory disease process occurring in middle-aged and elderly patients, predominantly affecting the intervertebral discs and facets joints. Narrowing of the spinal canal by osteophytic spurring produces myelopathy by compression of the spinal cord and radiculopathy by compression of the nerve roots. In this updated article, the author presents proper diagnostic criteria, presentation, differential diagnoses, pathophysiology, and treatment options, including the latest imaging criteria and a review of anterior and posterior surgical approaches.
|
• Cervical spondylotic myelopathy is an arthritic condition affecting the cervical facet joints and discs producing bony ridging in the central canal and neural foramina, resulting in compressive signs and symptoms of spinal cord and nerve root compression. | |
|
• Presenting features may involve a mix of upper and lower motor neuron dysfunction in the arms and hands, and upper motor neuron dysfunction in the legs. | |
|
• The diagnosis is established by combining clinical findings with the imaging characteristics of bony narrowing of the central and lateral aspects of the cervical spinal canal, as seen on MRI and CT. | |
|
• Treatment is directed at controlling arthritic axial neck pain, and surgical decompression with or without fusion is considered if signs and symptoms of myelopathy are present. |
Cervical spondylosis, often referred to as “hard cervical disc disease,” is a process involving a combination of degenerative changes in the intervertebral disc, the facet joints, and the ligamentum flavum. Cervical spondylotic myelopathy is the most serious consequence of this degenerative process, especially when associated with a congenitally narrow cervical vertebral canal (58). As Benzel has shown, spondylosis is a natural process of aging, is seen in 10% of individuals by the age of 25 years and in 95% by the age of 65 years, and is often preceded by mild segmental instability (16; 100). Dehydration of the disc leads to hardening and calcification with loss of disc resilience; ligamentous laxity provides a compensatory range of motion to the spine; the facet joints tend to enlarge to better share the stress loads, as the ligamentum flavum thickens in an attempt to stabilize the spine (35). The combination of these degenerative changes causing narrowing of the cervical spinal canal (spondylosis) and spinal cord injury (myelopathy) gives rise to the term “cervical spondylotic myelopathy.” It is technically not an arthritis, as degeneration of the intervertebral disc does not primarily involve the synovial membrane. Although the pathological existence of intervertebral disc herniation was realized as early as 1929 by Schmorl and Andrae (27), its clinical correlation with well-described syndromes of compressive myelopathy was not thoroughly reviewed until 1956, when only posterior decompressive surgeries were employed (27). Direct surgical attack on the anterior compressive disc-spur complex was not developed until the late 1950s with the work of Smith and Robinson (101) and Cloward (28). Cervical disc disease with progression to bony ridging and calcification of the posterior longitudinal ligament may occur anywhere in the cervical spine and over several levels, but most commonly is seen at C4-5, C5-6, and C6-7. Because it is a disease process, there is often a combination of stages of degeneration in the individual patient, such that one level may be predominantly a “soft disc” rupture and compression, whereas a more chronically degenerative level may exhibit “hard disc” compression. Either may be centrally located, causing spinal cord compression (myelopathy), laterally protruding into a narrowed foramen causing root compression (radiculopathy), or anterolateral with a mixed clinical picture of myeloradiculopathy.
Patients with cervical spondylosis usually present with neck pain with or without radiculopathy or myelopathy. Even painless progression of sensorimotor deficit is seen in patients with more centrally located compression, as the roots are relatively spared. Myelopathy develops in approximately 5% to 10% of patients with clinically symptomatic spondylosis (115), but cervical spondylosis is the most common cause of myelopathy in middle-aged and elderly patients (31; 79). It is rarely seen before the age of 40, and often no injury is elicited or the patient reports only a series of minor or repetitive strains.
Because cervical spondylotic myelopathy may involve compression of the descending lateral corticospinal upper motor neuron tracts and ascending dorsal column sensory tracts, as well as compression of the lower motor neuron in the central gray of the spinal cord, patients present with a variety of symptoms. Emphasis should be placed on obtaining a history of numbness and clumsiness in the hands, decreased fine motor movements, and subtle gait disorders. Suspicion of the clinical entity remains the single greatest element in early identification of cervical spondylotic myelopathy.
The clinical features, duration, and natural history of this condition vary considerably because of their relationship to the inconstant combination of mechanical, dynamic forces and periods of vascular ischemia (76). Consequently, various patterns of myelopathy have been described. Crandall and Batzdorf classified patients into five groups based on their dominant syndromes (31):
|
(1) The transverse syndrome involves the corticospinal, spinothalamic, and dorsal column tracts and produces severe spasticity, frequent sphincter involvement, and Lhermitte sign. | |
|
(2) The motor system syndrome involves the anterior horn cells and corticospinal tracts and produces marked spasticity but no sensory disturbances. | |
|
(3) The central cord syndrome produces severe motor and sensory disturbances with a greater expression of weakness in the upper extremities and spasticity in the lower extremities. | |
|
(4) The Brown-Sequard syndrome produces the typical contralateral sensory deficits and ipsilateral motor deficits. | |
|
(5) The brachialgia and cord syndrome involves the lower motor neurons of the upper extremities and produces radicular pain. |
Many patients also present with neck pain due to the degenerative components associated with spondylosis. Though patients may present with a radiculopathy secondary to extensive compression of various roots, it must be noted that cervical radiculopathy is not the main component of the disorder; long track dysfunction is the prerequisite of cervical spondylotic myelopathy. Similarly, a significant morbidity arising from cervical spondylosis is due to positional vertebral artery compression rather than spinal cord compression. A dramatic example of posterior circulation compromise due to cervical spondylosis can occur with therapeutic neck manipulation, or even with rotation-extension positions of the neck that may occur during sleep. An elderly patient awakening with acute nausea, vomiting, dysarthria, gait instability, and other signs of brainstem or cerebellar dysfunction should be studied urgently for cerebellar infarction due to cervical spondylotic vertebral artery compression (83).
Headache, or specifically “cervicogenic headache,” frequently accompanies neck pain in the spondylotic population, and one retrospective study found that approximately one third of patients suffered from chronic headache that was relieved in 43% of patients after anterior decompression with fusion (112). Another surgical study found again roughly one third of patients (50 of 166 cases) presenting with neurologic signs of spondylotic myelopathy suffered from chronic neck pains and headache and all patients undergoing anterior decompression with fusion noted significant relief of both neck pain and headache, the latter thought to be neuropathic in nature (89).
An additional presentation of cervical spondylotic myelopathy is posttraumatic central cord syndrome. In these patients, relatively minor trauma can precipitate a neurologically devastating injury. The pathophysiology is thought to involve vascular injury to the relatively poorly perfused medial regions of the cord from buckling of the hypertrophic ligament both anteriorly and posteriorly. Consequently, medial damage leads to preferential damage to the upper extremities. Early stages of spondylotic myelopathy with milder compression often present with hand numbness and complaints of impaired fine motor coordination in such tasks as buttoning a shirt or managing pills in a bottle. One group studying transcortical motor potentials and spinal cord sensory-evoked potentials during surgery found electrophysiologic evidence for this clinical progression, noting that the lateral part of the posterior funiculus mediating upper limb sensory function was more vulnerable to compression than was the lateral corticospinal tract (56).
The physical findings associated with cervical spondylotic myelopathy vary depending on the exact level of compression, the degree of compression modified by aggravating factors, and the span of segments comprised in the cervical spinal cord. Symptoms may be characterized by lower motor neuron involvement at the level of the clinical lesion and upper neuron involvement at the levels below the site of compression. Thus, lower extremity involvement will present with upper motor neuron symptoms, whereas the upper extremities may present with both upper and lower motor neuron involvement depending on the level and the nature of the compression. Clark proposed that the sensory findings in myelopathy usually include the loss of pain and temperature, proprioception, and vibrations below the level of the lesion, with the relative sparing of touch (26). These factors are clearly influenced by the multiplicity of levels and degrees of compression. The most common presentation is spastic weakness of the hands and forearms before involvement of the proximal upper extremity muscles and hand numbness with paresthesias, which may be painful. Wasting of hand musculature is a late finding and is often symmetric because of the central nature of osteophytic compression in the canal. Likely related to the compressive effect on lower motor neurons within the cord, mid-cervical spondylotic myelopathy may present with unilateral or bilateral hand weakness mimicking a C8-T1 radiculopathy (94). It is common for some patients to present with leg weakness, emphasizing the effect of long tract compression on lower extremity motor function. Typically, the proximal musculature is affected early, making it difficult for the patient to get up out of a chair, get out of a car, or climb stairs.
Reflexes are generally hyperreflexic below the level of compression and hyporeflexic at the level of the anatomic lesion because of impaired lower motor neuron function in the anterior horn. Pathologic reflexes, such as the presence of the Babinski reflex in the lower extremities and Hoffmann reflex in the upper extremities, characterize upper motor neuron involvement in the cervical spine. Furthermore, clonus may be present in the lower extremities. Lhermitte sign may be present when the patient flexes and extends the neck, producing a feeling of electrical shock. Lunsford and colleagues reported that although a significant number of patients manifest hyperreflexia (87%), only about 50% have the Babinski reflex and about 20% have the Hoffmann reflex (72). To further complicate the evaluation, it should be remembered that at least 10% to 20% of patients with cervical spondylosis have some degree of symptomatic lumbar stenosis as well, blunting the increased tone and hyperreflexia of the lower extremities produced by the upper spinal compression and adding radicular leg pain to the history (100).
Bladder and bowel symptoms tend to occur infrequently and late in cervical spondylotic myelopathy. Bladder dysfunction was demonstrated in 15% and bowel dysfunction in 18% of the patients in a clinical series of 269 patients with myelopathy (55). In a separate clinical study, Epstein and colleagues found that 20% of patients exhibited bladder dysfunction with various degrees of urinary retention (39). The most common urinary symptoms in early spondylotic myelopathy are urinary urgency and frequency, particularly in women. Impotence in males may occur with more chronic and severe cord compression but may have other causes in the older population.
Myelopathy hand, introduced by Ono and colleagues in 1987, is a loss of power of adduction and extension of the two ulnar fingers and an inability to rapidly grab and release these fingers (87). “Burning hand syndrome” from chronic vascular injury to the medial sensory tracts tends to be bilateral and symmetric, provoked by light touch that produces sustained burning. This is generally an indication of a late permanent hyperpathic sensory derangement that may respond little or not at all to surgical decompression.
Gait abnormalities are noticeable in patients with cervical spondylotic myelopathy. Gorter noted that cervical myelopathy usually presents initially as subtle gait disturbances with gradual deterioration (48). He stated that spasticity and paretic dysfunction occur first and are followed by numbness and a loss of fine motor movements in the upper extremities. A myelopathic gait with a hesitant, jerking motion may appear. In addition to the gait abnormalities, some patients present with lower extremity complaints that are more of a lower motor neuron involvement. This is not surprising because it is estimated that 5% of patients with cervical stenosis have concomitant lumbar stenosis (40). Treatment should first be directed toward the cervical component, which often improves or alleviates the lumbar component.
Though it has been several decades since the first clinical history of myelopathy was published, no definable natural history is available. Lees and Turner concluded clinical exacerbation added to neurologic deficits in patients with more than 10 years of myelopathy but emphasized that long periods of a neurologic stabilization occur between episodes of deterioration (68). Nurick supported this concept and concluded that the amount of disability in cervical myelopathy was established early in the disease process and generally did not progress significantly afterwards (86). Epstein's clinical review of 1355 patients with cervical spondylotic myelopathy determined in a conservative treatment evaluation that 36% showed improvement, whereas 64% showed no improvement (38). In the group that did not improve, 26% deteriorated neurologically with the remainders remaining stable. Sixty-seven percent of Symon and Lavender's patients displayed a linear relentless progression of neurologic deterioration rather than stabilization (103). A study classified patients who were “pre-symptomatic” with cervical spinal stenosis, followed them for a year, and determined that 19% had symptomatic progression; in 90% of these, an electrophysiologic data-based model was predictive (14).
Typically, patients with myelopathy have symptoms and signs for several years before seeking medical attention. Although the progression is usually slow, the course often involves a progressive decline if the disease is left untreated. A small percentage of patients exhibit a more rapid onset of progression of symptoms and signs.
Cervical spondylotic myelopathy is an intermittently progressive disease process without significant chance of reversal when no treatment is administered. Conservative therapy rarely solves the myelopathy. Once patients have presented with the signs and symptoms of cervical spondylotic myelopathy, most have some degree of permanent disability. Little chance of symptom resolution is possible with conservative treatment; therefore, patients with moderate or severe myelopathy are candidates for surgery. The two most important factors for successful outcome in patients treated for cervical spondylotic myelopathy are (1) the patient's age and (2) the duration of symptoms. Young patients tend to do better than elderly patients. With respect to duration of disease, patients whose disease has been present for fewer than 6 months have a more favorable outcome than patients whose symptoms have been present for 1 year.
Chiles and colleagues examined a group of 76 individuals after anterior decompressive surgery. Interestingly, improvement occurred in the lower extremities in 47% of patients compared to a 75% improvement in the upper extremities. Approximately 2% per year developed symptomatic restenosis at adjacent levels to the original decompression (25). A prospective multicenter study with independent clinical review was performed by Sampath and colleagues to analyze the outcome of patients treated for cervical myelopathy. The study, sponsored by the Cervical Spine Research Society, indicated that surgically treated patients had a significant improvement in functional status and overall pain, with improvement also observed in neurologic symptoms (95). Several radiological studies have shown that favorable prognosis following decompressive surgery of any type may be predicted by the severity of preoperative spasticity, weakness, and atrophy coupled with critical MRI spinal cord findings; patients with normal cord appearance or presence of intramedullary high-signal change on T2WI fare better than those patients with hypointense (low signal) change on T1WI, which may indicate permanent injury (03; 73).
A 56-year-old right-handed man presented with 3-year history of progressively severe radiating neck, right shoulder, and arm pain with intermittent paresthesias in both hands, right worse than left. Over the preceding 4 months, he had noticed impairment in fine motor coordination in his hands, with deterioration in his signature, difficulty with buttoning his shirt, and discriminating coins in his pocket. He also complained of fatigue and feeling of heaviness in his legs but without leg pain. He denied bladder or sexual difficulties. Physical exam revealed some loss of mechanical range of neck motion, particularly in rotation and in extension; Spurling maneuver provoked radiation of pain down the right arm from the shoulder with paresthesias in the entire right hand. Lhermitte sign was not elicited. Hoffman sign was present bilaterally. Mild weakness was noted in right biceps in forearm supination, right triceps, and finger extensors; grips were slightly weak, but abduction and adduction of both hands were moderately weak, right worse than left, with noticeable atrophy in right first dorsal interossei. Reflexes were diminished bilaterally in the upper extremities but brisk in the lower extremities. Gait appeared normal but with some difficulty with tight-roping. Lateral C-spine x-ray revealed a normally aligned but straightened spine with loss of normal lordotic curve, moderately severe spondylotic changes at the C5-6 disc space, narrowing with anterior and posterior spurring, and a chronically collapsed C6-7 disc space with more severe posterior spurring compromising the spinal canal.
Following surgery, he had almost immediate relief of pain and paresthesias in the right arm and both hands, with slowly improving strength in the proximal upper extremities. However, he had persistent weakness in hand intrinsics and lower extremity hyperreflexia at 1 year following surgery.
Although the cause of cervical spondylotic myelopathy has not been definitively pinpointed, four main theories for the development of this disease are available including: (1) a vascular hypothesis, (2) a compression hypothesis, (3) a hybrid of the first two (81), and (4) a dentate ligament theory (69). The cervical spinal cord receives its blood supply from the anterior spinal artery, paired posterior spinal arteries, and radicular arteries. Anastomoses are usually insufficient and occlusion of one radicular artery places the cord at risk for infarction. Within the ventral median fissure, the anterior spinal artery divides into short or proximal branches that supply the anterior funiculus and the central gray matter. The anterior spinal artery also is responsible for providing perfusion via long perforating branches that terminate in the lateral funiculus. The lateral cortical spinal tracts are supplied primarily by the long perforating branches with the medial portion of these tracts receiving additional supply from posterior spinal arteries and short perforating branches. The descending fibers of the cortical spinal tracts are arranged somatotopically. The fibers entering the upper extremities reside more medially, and the fibers responsible for innervating the lower extremity myelotomes are located more laterally.
After examining cross-sections of cadaveric spinal segments, Breig and colleagues noted that anterior posterior compression and compensatory lateral widening of the spinal cord compromise the longer perforating vessels (20). Therefore, ischemia secondary to compression may affect the lateral columns more than the anterior columns, explaining why the lower extremities are affected earlier and more severely than the upper extremities in cervical spondylotic myelopathy (81). Also supporting merit to the hybrid theory, Hoff and colleagues revealed a decrease in vessel filling within the gray and anterior lateral white matter in canines that had undergone compression followed by ischemia (52). In the last hypothesis, Levine showed that in a mechanical model of cervical spinal stenosis, tension transmitted from stretched dentate ligaments to the cord predicted patterns of injury typically seen clinically (69). Perfusion MRI scans confirm the final pathway of compression leads to spinal cord ischemia and hypoxia, resulting in permanent damage or “myelomalacia” (37).
Biomechanically, the intrinsic component of the human spine is the functional spinal segment. A functional spinal segment consists of the vertebral body with its intervertebral disc both superiorly and inferiorly. A component of this functional spinal segment is the 3-joint complex consisting of the intervertebral disc, the superior facet, and the inferior facet (41). As the human disc ages, it loses elasticity, disc space height, and the ability to distribute forces. These changes alter the force vectors of the posterior elements. Anular bulges increase mobility, and settling of the adjacent vertebral bodies results in buckling of the ligamentum flavum. Osteophytic spur formation occurs as an attempt to offset this increased dynamic mobility. Osteophyte formation provides stabilization between both adjacent vertebral bodies and increases the weight-bearing surface of the vertebral body endplates (19). Spurs that form anteriorly or anterolaterally rarely produce neurologic complications; however, if the spur evolves posteriorly or posterolaterally the neural foramen, the spinal canal, or both become compromised. This, coupled with facet hypertrophy, plays a dynamic role in narrowing the overall surface area of the cervical spinal canal.
The largest area of the cervical spinal canal is C1. From C2 distally, the cervical spinal canal funnels down, markedly decreasing the diameter for the cord. The normal cervical spinal canal from C3 to C7 is 17 mm to 18 mm in its sagittal diameter. Diameters of fewer than 12 mm have been found to be critical in the development of cervical myelopathy. Certain predisposing factors (ie, congenital spinal stenosis, ossification of the posterior longitudinal ligament, spondyloarthropathies, or trauma) also place some patients at a higher risk of developing symptoms. Two separate studies, Adams and Logue and Ono and colleagues, found a decrease in anterior posterior or sagittal components of the spinal canal in patients who develop cervical spondylotic myelopathy (01; 88). Mihara and colleagues performed a radiologic analysis of 18 elderly patients with C3-C4 spondylotic myelopathy in an attempt to elucidate the pathogenesis and concluded that two important features predispose the patients to the disorder of the cervical spine viz (1) greater C3-C4 angulation associated with age-related postural change and (2) hypermobility at the C3-C4 segment compensating for decreased mobility at the lower segments (77). A group studying patients with congenital cervical spinal stenosis had additional tendency toward disc degeneration as well as hypermobility of certain spinal segments, adding to the usual aging changes and leading to an earlier progressive myelopathy (80).
Some patients suffer from dynamic myelopathy. This syndrome consists of patients having few symptoms when maintained in the normal or flexed position, but marked exacerbation when the neck is extended, caused by buckling of the ligamentum flavum and posterior longitudinal ligament combined with osteophytic narrowing in hyperextension. One of the most dire events arising from spondylotic changes in the cervical spine in the elderly is seen in the cervical hyperextension fall; because of the underlying gait instability from proprioceptive loss, with or without spasticity, the patient lurches or stumbles forward, landing on the chest and chin with the head thrown back, acutely worsening the impact of the calcified disc and ligament against the cord. This often results in permanent quadriplegia, and, if the patient survives the fall, may be complicated by loss of cervical cord sympathetics as well, leading to severe bradycardia and hypotension; fluid resuscitation in this group of elderly patients with concomitant cardiac disease will lead to further deterioration from congestive heart failure, arrhythmias, and death.
Chronic cervical degenerative changes of the cervical spine are the most common cause of progressive spinal cord and nerve root deterioration (31). Ninety percent of men older than 50 years and of women older than 60 years display radiographic evidence of degenerative changes of the cervical spine (13). Increased recognition and treatment of cervical spondylotic myelopathy over the 10 year period from 1993 to 2002 has led the Stanford University group to report a doubling in patients admitted to U.S. hospitals with this disorder (from 3.73 to 7.88 per 100,000 admissions), and more than a 7-fold increase in its surgical treatment (from 0.6 to 4.1 per 100,000 admissions) (63). One study released from a nationwide database analysis in Taiwan that looked at patients hospitalized over a 12-year period for disabling signs or symptoms related to cervical spondylotic myelopathy noted that subsequent admissions for spondylotic myelopathy, as well as for spinal cord injury, were significantly higher among those patients treated conservatively than for those patients surgically treated (111). Potential genetic factors include those related to MMP-2 and collagen IX for degenerative disc disease and collagen VI and XI for ossification of the posterior longitudinal ligament (84). A 20-year Swedish study of construction workers found an increased risk for symptomatic cervical spondylosis and significant incidence of early retirement, particularly in jobs requiring prolonged spine load bearing and frequent or steady use of hands above shoulder height with neck in extension (57).
The only known prevention for cervical spondylotic myelopathy is maintaining nutritional health, avoiding cigarette smoking, which accelerates degenerative changes in the intervertebral disc, and attention to proper posture, including ergonomics in the workplace. All surgeons have encountered patients who have led relatively sedentary lives but have a “worn-out” neck from the secretarial habit of pinching a phone between ear and shoulder while writing or typing.
Beyond this, early recognition of the condition with surgical decompression can prevent a spinal degenerative process from resulting in a permanent neurologic syndrome.
Cervical spondylotic myelopathy usually affects patients over 50 years of age. Although the disorder is the most common cause of cervical cord dysfunction in the elderly, radiographic confirmation is warranted to confirm that an observed myelopathy is caused by cervical degeneration and not by another pathologic process. Cervical spine instability with canal compromise due to chronic subluxations is not uncommonly seen in the elderly patient and should be easily distinguished radiographically and by MRI. Similarly, C1-2 instability from rheumatoid pannus and chronic cervicomedullary compression may have a similar presentation. Other afflictions whose presentation may mimic cervical spondylotic myelopathy include disseminated sclerosis, multiple sclerosis, AIDS myelopathy, lupus myelopathy, A-beta-lipoproteinemia, B12 deficiency, tumors, syringomyelia, Chiari malformation, primary lateral sclerosis, and vertebrobasilar ischemia. Although cervical spondylotic myelopathy can frequently present as an isolated, painless, spastic lower paraparesis, if the imaging does not support a cervical compressive cause, the diagnostic work-up should aim higher. Chronic subdural hematoma and sagittal meningioma may produce this syndrome as well.
An important diagnosis to consider in the differential is amyotrophic lateral sclerosis, in which patients present with a combination of upper and lower motor neuron disease as well. It has been estimated that the diagnosis of amyotrophic lateral sclerosis is initially missed in nearly 40% of cases or that the signs and symptoms are attributed to another cause (96). However, the key differentiating factor is the region of lower motor neuron involvement--patients with cervical spondylotic myelopathy should only have cervical nerve root lower motor neuron symptoms and signs; patients with amyotrophic lateral sclerosis can have other lower motor neurons afflicted as well. To complicate matters, one study found nearly 48% of patients with amyotrophic lateral sclerosis have some degree of cervical spondylosis, with 8% undergoing surgery for progressive symptoms (113). Electromyographic findings, such as thoracic paraspinal muscle denervation preferentially in amyotrophic lateral sclerosis versus cervical spondylotic myelopathy, have been described as possible aids in differentiating diagnosis (62). Tongue atrophy and EMG evidence of tongue muscular denervation favors the diagnosis of amyotrophic lateral sclerosis. In addition, some cases of cervical myelopathy and concomitant canal stenosis with Chiari malformation have been reported in patients with fibromyalgia (51).
It may be difficult or impossible to distinguish between the relative contributions of cervical spondylosis and multiple sclerosis in producing myeloradiculopathy in the patient afflicted with both disorders. One series of 15 patients showed clear benefit of surgical decompression in reducing pain and paresthesias in the majority of cases, with many patients showing significant improvement in upper and lower extremity motor function; the surgeries were well tolerated (07).
Most middle-aged and elderly individuals suffering from spinal cord afflictions have some degree of degenerative changes of the cervical spine on imaging studies; therefore, a careful history and meticulous examination are essential for the accurate correlation of abnormalities observed with imaging and the patient's clinical picture. Plain radiographs including anterior, posterior, lateral, and oblique views should be obtained for patients with cervical spondylotic myelopathy. Flexion and extension radiographs are important for further evaluation of a patient with suspected cervical instability. Plain radiographs provide important information with respect to mass lesions, infection, trauma, and congenital abnormalities. The size of the spinal canal can be assessed, and anatomical landmarks can be identified that may be helpful for intraoperative localization.
However, plain radiographs do not provide an adequate assessment of soft tissue anatomy, the overall spinal column dimensions, or the spinal cord architecture. Prior to the advent of cervical MRI (C-MRI) in the mid-1980s, the gold standard for imaging cervical spondylotic myelopathy is CT following myelographic contrast into the intrathecal sac. As a result of the increase in the differential provided by the intrathecal material, better definition of a herniated disc or spondylotic ridge is provided when compared to CT or plain radiographs alone. In addition, intrathecal contrast provides an accurate assessment of the effect of the spondylotic ridge on the spinal cord itself. CT myelography also provides evaluation of the cross-sectional area of the cord and subarachnoid space, which may be of prognostic value. In a clinical review, Badami and colleagues found that patients with a cord to subarachnoid ratio of greater than 50% had good functional recovery after surgical decompression compared to those with less than 50% in whom no functional recovery was noted (09). The disadvantage of CT is that it exposes the patient to a formidable amount of radiation and requires a lumbar or cervical spinal tap, with the potential for the potential common complication (10% incidence) of postmyelographic headache and much rarer complication of nerve or spinal cord injury.
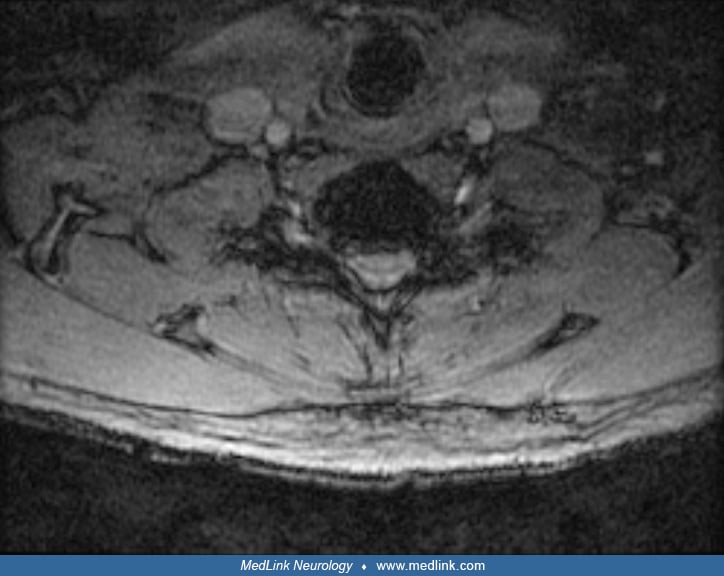
MRI allows the examination of the cervical spine for disc and spondylotic disease without exposing the patient to ionizing radiation or invasive myelography.
It provides excellent detail of the spinal cord, nerve roots, subarachnoid space, and soft tissue abnormalities (ie, soft disc herniation) and is preferred in assessing the presence of an intramedullary process and intradural or extradural neoplastic processes. A direct correlation has been demonstrated between degree of cord flattening on MRI scan and the delay in corticospinal motor conduction times as measured intraoperatively by transcranial magnetic stimulation (93). MRI may also provide prognostic value in patients undergoing operative decompression. In a study of more than 600 patients, 56% of patients whose MRI demonstrated increased signal intensity within the spinal cord on T2-weighted images, indicating spinal cord damage, had no improvement following decompression compared with 15% of patients with no abnormal signal (105). Matsumoto and colleagues tried to analyze the significance of increased signal intensity on T2-weighted MRI scans of the spine in the patients with cervical myelopathy to predict the outcome of conservative treatment. They concluded that increased signal intensity was not related to a poor outcome or the severity of the myelopathy (74). This is in contradistinction to a study by Papadopoulos and colleagues, who found that a 2-segment T2-hyperintense region was less likely to show improved outcome following decompression compared to a 1-segment hyperintensity or none present (90). MRI evidence of spinal cord swelling at or adjacent to the point of compression is often seen in younger patients and indicates a more rapid progression of spinal cord compromise, alerting to a more urgent need for decompression (104). Advances in MRI technology, such as diffusion tensor imaging, may find earlier changes of spondylotic myelopathy than with standard MRI imaging, especially when trauma from motion is suspected in cases showing significant bony canal stenosis without definite cord compression (11). The presence of gadolinium enhancement in the spinal cord behind the compressive anterior spur, often extending above and below the point of compression for one or more segments, can be confusing to the clinician who is concerned that the patient may have a separate process affecting the cord, such as transverse myelitis or intramedullary tumor. A Mayo Clinic study retrospectively studied 56 patients who underwent surgery for spondylosis over a 16-year period who presented with cord enhancement on MRI and noted that despite overall improved outcome the enhancement usually persisted for months or years after decompression. The critical point is that as many as 70% of patients were initially diagnosed with inflammatory or neoplastic intramedullary cord disease, rather than attributing the enhancement to compressive spondylosis, and had a delay in surgical treatment for an average of 11 months; biopsy of the spinal cord in six instances failed to yield a diagnosis other than compressive myelopathy (44).
Diffusion tensor imaging (DTI) MRI may come to replace or supplement conventional MRI in the evaluation of early cervical spondylotic myelopathy because of greater sensitivity for white matter edema or injury (82; 108; 02; 70).
Flexion-extension MRI is also gaining favor with the global neurosurgical community, as studies have shown an increased sensitivity for detecting cord compression using dynamic imaging, as well as a change in surgical approach with the additional dynamic information compared with use of static neutral MRI alone (06).
One option to better define the bony anatomy for measuring canal size, evaluate the quality of previous fusion areas, and determine the size of pedicles and location of the vertebral artery foramina for surgical planning is a thin-section cervical CT (C-CT). This study avoids the risks and patient discomfort of a myelogram and, coupled with C-MRI, will usually suffice for preoperative evaluation. C-CT also has the advantage of distinguishing ossified posterior longitudinal ligament from the simple calcifications of cervical spondylosis and clarifying the extent of ossified posterior longitudinal ligament for purposes of surgical planning.
One study looking perioperatively at patients with cervical spondylotic myelopathy with positron emission tomography showed characteristic changes in the cervical cord prior to surgery, which may help to indicate which patients will benefit from surgical decompression (36).
Ideally, cervical spondylotic myelopathy is a surgically treated entity, but certain patients present an unacceptable risk, frequently pulmonary or cardiac, for general anesthesia and surgical intervention. Attention is then directed at medical management of chronic arthritic and neuropathic pain, spasticity, and associated bladder dysfunction as indicated (75). These techniques are frequently effective in management of the postoperative patient with residual symptoms.
Advances in spinal imaging and accumulation of clinical experience have provided some clues as to indications and timing of surgery for cervical myelopathy. Yonenobu suggested the duration of myelopathy prior to surgery and the transverse area of the spinal cord at the maximum compression level as the most significant factors influencing the decision to perform surgery (114). When surgery is properly carried out, long-term results are expected to be good and stable. Surgery to relieve the compression may reduce the pain and disability, though it is associated with a small but definite risk. The short-term effects of surgery, in terms of pain, weakness, or sensory loss, have been proven to be superior (45). Surgery for asymptomatic elderly individuals with imaging evidence of cord compression, performed as a preventive measure, is controversial. One study in the Czech Republic showed a low incidence of spinal cord injury from minor trauma in patients identified with asymptomatic spondylotic canal compromise, so recommended management has been simple risk avoidance in this group (15).
An Italian group has used advanced MRI imaging techniques to determine the role of neuronal plasticity in functional recovery after cervical cord decompression in patients with compressive myelopathy. Using diffusion MRI and functional MRI, they found cortical and subcortical areas undergoing neuronal reorganization that was consistent with findings also seen during recovery after spinal cord injury (17). Analysis of the literature regarding spondylotic myelopathy does not demonstrate conclusively the superiority of either the anterior or the posterior approach (23); however, no true comparative prospective trial has ever been established. Instead, successful surgery depends on proper patient selection and selection of the approach that provides optimal decompression of the spinal cord. As a general rule, the anterior approach is appropriate for patients whose pathological compression occurs anterior to the spinal cord at three or fewer vertebral segments. For most patients with cervical disc disease or spondylosis, the compression lesion lies anterior to the spinal cord. For this reason, it is felt that the anterior approach provides more thorough and complete decompression. Also, for patients whose preoperative lateral cervical spine reveals a kyphotic deformity, the anterior approach is mandated for cervical decompression because a posterior approach could exacerbate the kyphosis, worsening the myelopathy.
The two most common anterior approaches for discectomy are (1) the Cloward technique and (2) the Smith-Robinson technique. The Smith-Robinson technique replaces the removed intervertebral disc and osteophytic bar with a tricortical horseshoe-shaped graft. Initially this was provided by harvesting a tricortical wedge from the patient’s iliac crest. Over the past two decades, this technique has been replaced by bone from other sources, including allograft iliac crest and machined corticocancellous allograft spacers that can achieve comparable fusion rates as autograft, particularly with the availability of fusion “enhancers” such as demineralized allograft bone matrix. The introduction of anterior cervical plating systems has also improved postoperative alignment and fusion by supporting the fusion construct with a more even distribution of forces on the grafts and the patient’s own bone. In the Cloward technique, the superior and inferior end plates as well as the intervertebral discs are removed in a circular fashion, and the removed segments are replaced with a round dowel graft. In order to achieve adequate decompression, the posterior osteophytic bar must be resected regardless of technique performed. Removal of the degenerated posterior longitudinal ligament in each case is recommended, as it is typically thickened and calcified and directly impacts the ventral dura in the majority of cases (10).
Bone grafting is an adjuvant in the treatment of cervical spondylotic myelopathy via the anterior approach. Though previous studies (49) have shown that no difference exists in single level fusion versus no fusion, others (97) have advocated that bone grafting alleviates immediate postoperative pain and helps prevent further kyphosis that may render the spinal cord more compressed, worsening the myelopathy. Regardless of the technique used, patients should have some type of bone grafting procedure performed to eliminate kyphosis at the level of fusion. Preferred options for interbody fusion materials include iliac crest or fibular strut autograft, cadaver allograft, and titanium or PEEK (polyetheretherketone) cage packed with demineralized bone matrix (DBM) or recombinant bone morphogenic protein (BMP). PEEK cages have the advantage of modulus of elasticity similar to bone, allow minimal subsidence during the months of ongoing fusion, and, thus, maintain the restored foraminal and disc space height and lordosis achieved at surgery (61; 34).
Review of the literature supports the use of stacked anterior interbody fusion cages over three and four levels as a satisfactory method for cord decompression, fusion with restoration of cervical lordosis, and minimal associated dysphagia and dysphonia (04; 05). Advisories against use of BMP in anterior cervical fusion have been issued based on a significant incidence of postoperative soft tissue swelling, dysphagia, and even fatal airway obstruction; this complication is likely dose-dependent, and further studies are needed to determine safety of BMP in this context (109; 107). The advantage of maintaining or restoring motion after anterior decompression of the cord by placement of prosthetic cervical disc has not been established in the generally older spondylotic population; the real or theoretical risk of accelerated adjacent segment disc deterioration following fusion is more a concern for the younger, more active patient with soft disc rupture (98). A large metaanalysis of over 60,000 patients (20 years of age or greater) undergoing anterior cervical fusion and followed for 11 years found an average of 6.57% symptomatic adjacent segment disease requiring additional level fusion surgery, with the highest group requiring additional surgery at 8.12% among those 30 to 39 years of age with those undergoing initial multilevel surgery (99).
Regarding the relative benefits of fusion versus arthroplasty, a 5-year prospective randomized trial comparing 99 patients randomized to either single-level disc arthroplasty or anterior cervical interbody plated fusion found a higher incidence (seven patients) needing additional surgery for adjacent segment disease in the fusion group as compared with the disc arthroplasty group (one patient) (54). Additional studies comparing single or multilevel arthroplasty for cervical spondylotic myelopathy with anterior decompression (discectomy or corpectomy) fusion surgery have shown equal safety and satisfactory improvement in neurologic deficits and symptoms (117; 30; 50). Although there is a risk of nonunion with any fusion surgery, one study suggested that the time for achieving fusion may be quite protracted in this elderly group, following nine nonunion patients of 31 total who had failed to achieve radiographic fusion at 2 years, with five of those going on to fuse at between 3 and 6 years postoperatively; they found no pain scale correlation between those with fusion and those with nonunion, and the majority all had significant axial pain resolution over the time observed (65). A Taiwan group published an unusual series of 4-level cervical disc arthroplasty for multilevel cervical spondylosis, justifying this approach on the fact that some degree of pseudoarthrosis on one or more levels is likely when attempting interbody fusion; 20 patients were studied with a 3-year follow-up, and they found preserved or improved cervical mobility with minimal complications (24).
Multiple anterior discectomies with resection of associated osteophyte in spondylotic myelopathy may not allow adequate visualization and resection of the compressive complex; significant spurring may be left against the cord behind the vertebral bodies above and below one or more disc spaces. For this reason, anterior medial corpectomy with strut grafting, or interbody cylinders of titanium, carbon fiber, or PEEK packed with autologous, synthetic, or allograft bone may be recommended for patients whose compression spans multiple herniated disc segments. This approach allows complete removal of the anterior cord impingement, creates a stable spine, and may avoid the pseudarthrosis that can occur with multiple level grafts in the elderly, osteoporotic patient.
Fessler and colleagues performed multilevel corpectomy and fusion with or without instrumentation in 93 patients (43). Symptomatic improvement was seen in 92% of patients, and there was a complication rate of 18% (43). Whether performed as one or more anterior discectomies or as a corpectomy, the specific risks of the anterior approach include spinal cord injury as well as failure to adequately decompress the spinal cord, nerve root injury and dural tear with spinal fluid leak, injury to soft tissues dissected (esophagus, carotid sheath structures), injury to the recurrent laryngeal nerve and vocal cord paralysis, sympathetic chain injury (Horner syndrome), hematoma formation with compromise of airway or spinal cord, infection, and failure to achieve fusion. More studies are coming out advocating the use of polyetheretherketone (PEEK) cages in place of allograft bone, demonstrating comparable rates of fusion in elderly patients while avoiding reliance on bone bank materials (60). Postoperative anterior wound hematoma or seroma was found to be the most common surgical complication requiring early (within 30 days) readmission in over 45,000 Medicare patients, with an incidence of 1% to 1.4% (92). One disadvantage of the corpectomy approach is the straightening of the spine that results in replacing two or more spinal segments with a single strut graft; one evenly divided study of 100 patients showed improved preservation of cervical lordosis with a multilevel interbody fusion technique versus “hybrid” technique of corpectomies with strut construct (22).
Thorough decompression of the spinal cord can be achieved through the individual space; corpectomy is not required, and total disc replacement (disc arthroplasty) has been advocated and used effectively at one or more levels to maintain alignment and preserve mobility, with reports of equal outcome to anterior discectomy with fusion procedures (91; 33; 21).
Vertebral body sliding osteotomy is a variation of an anterior surgical decompression technique in which cuts are made through the lateral aspect of each of the vertebral bodies at the level of cord compression by osteophytic disc or ossification of the posterior longitudinal ligament (OPLL), and the middle core of each vertebral body is lifted anteriorly—away from the anterior spinal cord—and secured with an anterior plating system (67; 66). In addition, adjacent segments above and below the levels of compression also undergo discectomy with implant and plated fusion so that lordosis can be restored. The technique reportedly has a lower rate of dural tear with improved fusion rates and better sagittal alignment than with corpectomy and strut graft fusion.
Posterior techniques are performed in patients whose pathologic compression encompasses more than four vertebral body segments, and for those patients in which the posterior canal compromise by thickened ligamentum flavum, overgrown facet joints, or congenitally short pedicles is as great as or greater than the anterior compression elements. The two techniques used for posterior decompression include cervical laminectomy with or without lateral mass plating or laminoplasty. Though both techniques allow for adequate posterior decompression, laminoplasty was developed to help maintain posterior stability and prevent postoperative laminectomy kyphosis, which can worsen cervical myelopathy. The goal of operative intervention for cervical spondylotic myelopathy is to provide adequate decompression; thus, the adequate width of the laminectomy or laminoplasty must be to either side of the cervical spinal cord dura. This allows complete and thorough decompression without injuring the facet joints and potentially provoking or worsening any preexisting instability. The incidence of postlaminectomy kyphosis—“swan neck deformity”—done without fusion has been reported at 21% (102) but may be less in those patients who present with adequate cervical lordosis before surgery. A Swedish group followed 60 patients treated with posterior laminectomy alone for 8 years and noted no significant change in degree of lordosis over time (71). Several groups have shown no long-term benefit to laminoplasty over simple laminectomy for patients presenting without loss of lordosis or gross instability (110). Multilevel laminoplasty tended to generate more chronic axial pain without significant reduction in long-term straightening or kyphosis (85). A metaanalysis from the Netherlands showed no significant benefit of laminoplasty over laminectomy with or without fusion, and a higher complication rate for laminoplasty (12). Surgeons in South Korea reached the same conclusion by a seven-study metaanalysis of nearly 600 patients evenly distributed between the two procedures (64). Delayed interlaminar fusion with increased kyphosis has been reported after laminoplasty with longer postoperative follow-up (59). Lateral mass plating has virtually eliminated the need for cervical laminoplasty in the adult spine, as it achieves a high rate of fusion without risk of recurrent canal compromise (53; 29). Another successful surgical technique for posterior decompression fusion using bilateral facet cages has been reported (18). One group reported 81% improvement in myelopathy over 17 months of postoperative recovery in 54 consecutive patients undergoing laminectomy and instrumented fusion, with the remainder of patients halting progression of their symptoms (47). Another group measured significant posterior drift of the spinal cord away from anterior spurs following successful laminectomy with instrumented fusion, further recommending this treatment approach (106). One benefit cited for the posterior decompression, instrumented fusion approach is postoperative resorption of anterior compressive spurring, as measured by MRI scanning (08). Specific risks of the posterior approach for spinal cord decompression include spinal cord injury or failure to adequately decompress the spinal cord, dural tear with spinal fluid leak, instability and late kyphosis, infection, hemorrhage, and hematoma formation, and combined with posterolateral fusion, nerve root and vertebral artery injury, and failure to achieve fusion. A Chicago group published favorable preliminary data on patients undergoing minimally invasive endoscopic decompression without fusion for cervical spondylotic myelopathy, with good outcomes and reduced morbidity compared to the more extensive muscle dissection and hardware placement required for the open surgical techniques (32). In general, according to extensive meta-analysis of the literature, if anterior decompression with fusion can be tolerated by the patient and still achieve satisfactory spinal cord decompression, it is felt to be better than the posterior approach, with less operative and long-term morbidity (78).
In summary, assuming a well-chosen approach and method for decompression, with or without fusion, surgery is strongly recommended as the preferred treatment, as supported by a prospective international study of 479 patients (42). Most comparative studies favor surgery tailored to the specific anatomy of compression and the tolerances of the individual patient rather than to an anterior or posterior approach for all (116; 46).
Positioning patients with cervical spondylotic myelopathy during intubation is extremely important. Hyperextension, which occurs frequently during intubation, can narrow the cervical spinal canal and further compromise the already damaged cervical cord. Consequently, intubation should be performed with the neck in neutral position, with or without fiberoptic intubation; occasionally awake fiberoptic innervation is advisable. Motor and sensory evoked potential monitoring can add an additional layer of protection to the patient and comfort to the surgical team and, if used, should be initiated prior to turning when the posterior approach is used. Loss of evoked potentials during positioning can be instructive and prompt immediate attention to neck position as well as blood pressure and adequate spinal cord perfusion. It is imperative that the anesthesiologist provide adequate perfusion to the compressed spinal cord, particularly during the decompression, with proper fluid management and avoidance of hypotension. For this reason, the sitting position is contraindicated for surgery on the patient with spondylotic myelopathy.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Saul S Schwarz MD
Dr. Schwarz of the University of Colorado Health Sciences has no relevant financial relationships to disclose.
See Profile
Randolph W Evans MD
Dr. Evans of Baylor College of Medicine received honorariums from Abbvie, Amgen, Biohaven, Impel, Lilly, and Teva for speaking engagements.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
General Neurology
Jan. 13, 2025
General Neurology
Jan. 13, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 08, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 07, 2025
General Neurology
Dec. 30, 2024
General Neurology
Dec. 13, 2024
General Neurology
Dec. 13, 2024
Neuromuscular Disorders
Dec. 09, 2024