General Neurology
Use of focused ultrasound in neurologic disorders
Jan. 13, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Cardiac arrest is defined as the cessation of cardiac activity as confirmed by the absence of signs of circulation. Out-of-hospital cardiac arrest incidence and outcomes vary greatly around the globe. During cardiac arrest, basic CPR and early defibrillation are of primary importance. The COVID-19 epidemic has adversely impacted the epidemiology, diagnosis, management, and outcome of cardiac arrest. Preceding acute respiratory insufficiency is generally responsible for COVID-19-associated in-hospital cardiac arrest, and patients with COVID-19 who received cardiopulmonary resuscitation after in-hospital cardiac arrest have low survival rates. Reports have indicated that the incidence of out-of-hospital cardiac arrest and in-hospital cardiac arrest have significantly increased. Chances of survival in cases of out-of-hospital cardiac arrest are poor; however, patients with in-hospital cardiac arrest have a better chance of survival. Therapeutic hypothermia increases the chances of survival and reduces the risk of neurologic damage following cardiac arrest. Prognostic determination of patients in coma after resuscitation from cardiac arrest is a common and difficult requirement with significant ethical, social, and legal implications. Several studies have suggested the usefulness of clinical examination, electrophysiologic studies, biochemical markers, and neuroimaging in predicting poor neurologic recovery in comatose survivors. Diffusion tensor magnetic resonance imaging accurately predicted neurologic outcomes in patients who were unconscious after cardiac arrest. Five clinical signs were found to strongly predict death or poor neurologic outcome: absent corneal reflexes at 24 hours, absent pupillary response at 24 hours, absent withdrawal response to pain at 24 hours, no motor response at 24 hours, and no motor response at 72 hours. Short latency somatosensory evoked potential N20 is now a well-accepted predictor of poor prognosis. Neuroimaging may reveal extensive cortical and subcortical brain atrophy. The anatomical regions that are more significantly affected include the frontal cortex, posterior cingulate cortex, thalamus, putamen, pallidum, caudate, hippocampus, and brain stem. Bystander and first responder resuscitation are crucial. Bystander-initiated cardiopulmonary resuscitation is associated with a greater likelihood of survival with good outcome. Prehospital resuscitation efforts should be done for at least 40 minutes in bystander-witnessed out-of-hospital cardiac arrest. Mechanical chest compression devices are satisfactory alternatives. However, mechanical chest compression devices are only to be used when manual chest compressions are impractical, impossible, or unsafe. Chances of favorable neurologic recovery are higher following immediate coronary angiography, with or without percutaneous coronary angioplasty. Sodium bicarbonate administration is frequently administered to counteract acidosis. Several machine learning models are proving valuable in predicting prognosis after cardiac arrest. Random Forest and Convolutional Neural Networks were the best for predicting postcardiac arrest neurologic outcomes from EEG data, with potential improvement when combined with health records. In this article, the author discusses in detail the various aspects of prognosis after cardiac arrest.
|
• Cardiac arrest is the cessation of cardiac activity as confirmed by the absence of signs of circulation. | |
|
• Sudden cardiac death from cardiac arrest is the most common cause of death. | |
|
• Cardiac disorders like coronary heart disease, cardiomyopathies, cardiac arrhythmias, congenital heart diseases and valvular heart diseases predispose a cardiac arrest. | |
|
• Clinical examination, electrophysiologic studies, biochemical markers, and neuroimaging help predict recovery in comatose survivors. | |
|
• Five early clinical signs that predict poor outcome include absent corneal reflexes, absent pupillary response, absent withdrawal response to pain, and no motor response. | |
|
• Therapeutic hypothermia has considerably improved outcomes after adult cardiac arrest. |
Sudden cardiac death from cardiac arrest is the most common cause of death worldwide. Efforts are ongoing to find ways to improve the ability to revive patients in cardiac arrest and to limit damage following cardiac arrest.
In 1740, The Paris Academy of Sciences officially recommended mouth-to-mouth resuscitation for drowning victims. In 1891, Dr. Friedrich Maass, a German surgeon, performed the first equivocally documented chest compression in humans. George Crile, Chief of Surgery at Western Reserve University was the first to successfully use external chest compression in 1903 and the first to use adrenaline (epinephrine) in resuscitation in 1909. Kouvenhoven and coworkers reported the results of chest compression on 20 patients, of whom 14 were successfully revived (33). Dr. Claude Beck, professor of cardiothoracic surgery, performed the first successful human cardiac defibrillation in 1947 (76). In 1956, Peter Safar and James Elam first documented the adequacy of mouth-to-mouth resuscitation (68).
Hippocrates suggested in 450 BC that packing patients in snow might have benefit to survival. In the November 1950 Annals of Surgery, Bigelow and coworkers described the possible role of hypothermia on the basis of their experiments on dogs (09). The New England Journal of Medicine in 2002 published a landmark paper documenting unequivocally the role of hypothermia in cardiac arrest (07).
Pennsylvania state legislators passed “House Act 59, Sudden Cardiac Arrest Prevention Act,” in August of 2012; the intent of this law was to educate children, parents, and coaches about the symptoms that are associated with sudden cardiac death.
Cardiac arrest is the cessation of cardiac mechanical activity as confirmed by the absence of signs of circulation. Historical details of a cardiac arrest event should always be obtained from a witness. It is essential to establish the possible underlying cause of the catastrophic event. History of cardiac symptoms, such as chest pain, breathlessness, and palpitations, may suggest a cardiac cause.
Cardiac arrest usually happens without any warning signs. The initial clinical feature of sudden cardiac arrest is loss of consciousness. Neurologic dysfunctions among survivors of cardiac arrest are predominantly alterations in consciousness. In the most severe cases, coma may be irreversible or evolve as a minimally conscious state, a vegetative state or even brain death. Other manifestations include seizures, myoclonus, and status epilepticus. Early myoclonus in comatose survivors of cardiac arrest is a sign of severe global cerebral damage and has been associated with poor prognosis (44).
Despite advances in the treatment of heart diseases, the outcome of patients experiencing cardiac arrest remains poor. In the United States, the overall survival rate to hospital discharge is approximately 10%. For 31,689 out-of-hospital cardiac arrest events reported in the United States between 2005 and 2010, approximately 22% of patients were pronounced dead after resuscitation efforts were terminated in the prehospital setting. The survival rate to hospital admission was 26%, and the overall survival rate to hospital discharge was around 9.6% (46). Japan has experienced significant improvement in the prognosis of out-of-hospital cardiac arrest over the years. Bystander cardiopulmonary resuscitation and defibrillation are associated with lower risks of brain damage and death from any cause as compared with no bystander resuscitation (67; 35).
In a Japanese study spanning 5 years (2005 to 2009), 547,153 overall out-of-hospital cardiac arrest patients and 169,360 bystander-witnessed out-of-hospital cardiac arrest patients were enrolled (31). The main outcome measure of this study was 1-month survival with favorable neurologic outcome. Neurologically favorable survival significantly increased from 1.6% in 2005 to 2.8% in 2009 among overall out-of-hospital cardiac arrest. In addition, among bystander-witnessed out-of-hospital cardiac arrest and bystander-witnessed ventricular fibrillation out-of-hospital cardiac arrest, neurologically favorable survival increased from 2.1% to 4.3% and from 9.8% to 20.6% respectively. Public-access automated external defibrillator use, either bystander-initiated chest compression-only CPR or conventional CPR, and earlier emergency medical services response time were associated with a better neurologic outcome.
Survival after in-hospital cardiac arrest is much better than out-of-hospital cardiac arrest. According to 2014 data from the United States, among 93,342 adults with an in‐hospital cardiac arrest at 231 hospitals, the mean unadjusted hospital survival rate was 18.2% (23).
A similar survival rate for in-hospital cardiac arrest has been recorded in the United Kingdom as well. Among 22,628 patients aged 16 years or older who received chest compressions and/or defibrillation and were attended by a hospital-based resuscitation team in an in-hospital setting, overall survival to hospital discharge was 18.4%. The presenting rhythm was shockable (ventricular fibrillation or pulseless ventricular tachycardia) in 16.9% and nonshockable (asystole or pulseless electrical activity) in 72.3%; rates of survival to hospital discharge associated with these rhythms were 49.0% and 10.5%, respectively (56).
Long-term outcome after cardiac arrest is generally poor, and survivors have considerably lower quality of life (71). Schnaubelt and colleagues interviewed 178 patients with survival times ranging from 4.2 to 12.6 years. Authors noted that the favorable factors determining prolonged survival were younger age, female sex, and shorter duration of hospitalization and coma. The factors that were found responsible for lower quality of life among these survivors included poor mobility, poor self-care, or persistence of pain.
In a study among patients with perioperative cardiac arrest, one in three survived to hospital discharge, and good neurologic outcome was noted in two of three survivors (65). The authors included patients aged 18 years or older who experienced an index, pulseless cardiac arrest in the operating room or within 24 hours postoperatively. The primary outcome was survival to hospital discharge, and the secondary outcome was neurologically intact recovery among survivors. A total of 2524 perioperative cardiopulmonary arrests were identified from 234 hospitals. The overall rate of survival to discharge was 31.7%, including 41.8% for ventricular tachycardia and ventricular fibrillation, 30.5% for asystole, and 26.4% for pulseless electrical activity. Ventricular fibrillation and pulseless ventricular tachycardia were independently associated with improved survival. At discharge, the rate of neurologically intact survival was 64.0%. Pre-arrest neurologic status at admission, patient age, inadequate natural airway, pre-arrest ventilatory support, duration of event, and event location were significant predictors of neurologic status at discharge.
After cardiopulmonary resuscitation (CPR), a large number of patients remain unconscious even after circulatory status is restored. Severe anoxic damage of the brain causes coma in these patients. Brain damage may happen during resuscitation. In some patients, restoration of sensorium usually takes place within a few days after resuscitation. Neurologic impairment is expected if a patient fails to regain consciousness rapidly; the majority of survivors are left with severe disability and are often completely dependent on others for basic needs of life. Prognostic assessment of patients who are in coma after resuscitation from cardiac arrest is often crucial but difficult. Zandbergen and colleagues, in a multicentric study, prospectively evaluated 407 patients (who were unconscious 24 hours after CPR) for the assessment of prognosis (86). Poor outcome was defined as death or persistent vegetative state 1 month after CPR. The authors noted a poor outcome in 356 (87%) of the patients, 349 of whom died later. Of the remaining 51 patients who were conscious after 1 month, 34 were severely disabled and 10 were moderately disabled. Only seven patients were able to make a good recovery. Of the 34 patients who were severely disabled after 1 month, 11 had died after 1 year, 13 remained severely disabled, and 10 had become independent.
Prognosis following therapeutic hypothermia. In a landmark paper, Bernard and coworkers documented efficacy of moderate hypothermia in patients with coma after resuscitation from out-of-hospital cardiac arrest. In a randomized study, 49% of patients (21 of 43) who were treated with hypothermia survived and had a good outcome--that is, they were discharged home or to a rehabilitation facility--as compared with 26% (9 of 34) treated with normothermia (07). The latest Cochrane meta-analysis suggested that mild therapeutic hypothermia seems to improve survival and neurologic outcome after cardiac arrest (01). This review included four trials and one abstract reporting on 481 patients. Patients in the hypothermia group were more likely to achieve a score of 1 or 2 on the best cerebral performance categories scale (5-point scale: 1 = good cerebral performance; 5 = brain death) during the hospital stay and were more likely to survive to hospital discharge compared to standard post-resuscitation care. Another review also suggested that the use of mild therapeutic hypothermia for 24 hours in comatose patients resuscitated from nonventricular fibrillation or ventricular tachycardia arrest was associated with a 15% reduction in hospital mortality and significant improvement in neurologic outcome (69).
Target body temperature during hypothermia therapy is controversial. In one trial involving unconscious survivors of out-of-hospital cardiac arrest, hypothermia at a targeted temperature of 33°C was not found beneficial compared with a targeted temperature of 36°C (55). The objective of the study was to compare two target temperatures, both of which were intended to prevent fever. A total of 939 patients were included in the study. At the end of the trial, 50% (235 of 473) of the patients in the 33°C group had died as compared with 48% (225 of 466) of the patients in the 36°C group.
Prognostic indicators of neurologic recovery. Several studies have suggested the usefulness of clinical examination, electrophysiologic studies, biochemical markers, and neuroimaging in predicting poor neurologic recovery in comatose survivors after CPR (21). Booth and coworkers, in their study, reviewed all available literature and tried to determine the predictive accuracy of bedside clinical examination in establishing prognosis of post-cardiac arrest coma (10). Five clinical signs were found to strongly predict death or poor neurologic outcome: (1) absent corneal reflexes at 24 hours, (2) absent pupillary response at 24 hours, (3) absent withdrawal response to pain at 24 hours, (4) no motor response at 24 hours, and (5) no motor response at 72 hours. It was suggested that simple physical examination could accurately predict death or poor outcome in these patients. The most useful assessment was possible at only 24 hours after cardiac arrest.
Young and coworkers studied 75 comatose patients resuscitated from cardiac arrest, excluding those who were brain dead or continuously sedated (84). Clinical examinations were performed on day 1. The following proportions of patients recovered awareness: 2 of 18 patients with absent pupillary reflexes; 18 of 57 with preserved pupillary reflexes; 2 of 32 with absent corneal reflexes; 16 of 43 with preserved corneal reflexes; 0 of 15 with absent oculovestibular reflexes; and 8 of 29 with preserved oculovestibular reflexes. Purposeful movements were associated with a high probability of recovery, whereas other categories were unfavorable. Other categories of motor response were associated with an increased proportion of those who died without recovering awareness, but each category had some survivors. American Academy of Neurology practice parameters also observed that clinical features like pupillary light response, corneal reflexes, motor responses to pain, and presence of myoclonus status epilepticus are reliable predictors of poor outcome in comatose patients revived by CPR (83).
Loss of the N20 component of median somatosensory evoked potentials is considered a reliable indicator of unfavorable prognosis in post-cardiopulmonary arrest patients. Bilateral absence of early cortical responses of the somatosensory evoked potentials (N20) in the first week after CPR is considered to have 100% specificity. In a large prospective cohort study comprising 407 adult patients who were unconscious 24 hours after CPR, early cortical responses (N20) were evaluated at 24, 48, and 72 hours (86). Poor outcome was defined as death or persistent vegetative state 1 month after CPR. Absent N20 indicated a 0% false-positive test rate in predicting poor outcome. In another study, somatosensory evoked potentials were recorded in 47 patients (84). One of 21 patients with loss of the N20 component survived compared with 11 of 26 patients in whom N20 was recorded. As a matter of fact, in patients who remain in coma days after CPR and do not elicit brainstem reflexes, even normal electrophysiologic patterns do little to alter the overall prognosis (32). Electroencephalography can be performed during therapeutic hypothermia or shortly thereafter; continuous or reactive electroencephalography background strongly predicts good recovery from cardiac arrest. On the contrary, unreactive or spontaneous burst-suppression electroencephalography pattern, together with absent N20 on somatosensory evoked potentials, is almost 100% predictive of irreversible coma (57). Some data also suggest that somatosensory evoked potentials predict poor neurologic outcome. A cohort of 262 patients (83 in the good outcome group and 179 in the poor outcome group) was analyzed (59). A bilaterally absent N20 was found in 127 patients and predicted a poor outcome with a sensitivity of 71%; among the patients with absent brainstem reflexes (n = 103), three had a good outcome. The absence of one or both N20 and brainstem reflex had a sensitivity of 84.2% (59).
Among biochemical markers, a serum neuron-specific-enolase level greater than 33 microgram per liter has been identified as another reliable prognostic indicator in patients revived by CPR (47). In one study, during the first 7 days after CPR, median values of neuron-specific-enolase and S-100B were found increased in patients who remained unconscious after CPR compared to those patients who regained consciousness (87). In another study, serum neuron-specific-enolase concentrations were serially determined in 227 consecutive unconscious patients after CPR. Poor neurologic outcome was indicated in 33% of 177 analyzed patients. A peak neuron-specific-enolase concentration above 80 ng/ milliliter predicted persistent coma at specificity of 100% with a sensitivity of 63% (66). In a systematic review and meta-analysis, Sharma and colleagues noted that higher neuron-specific-enolase values (70.4 ng/mL at 24 to 48 hours and 58.6 ng/mL at 48 to 72 hours) had better predictability of poor outcome (73).
Blood gas (PaO2 and PaCO) data obtained within the first 24 hours in comatose adult patients do not predict outcome after cardiac arrest. In a cohort 356 patients the highest and lowest PaO2 and PaCO2 were similar in patients with unfavorable and favorable neurologic outcomes (62).
A meta-analysis revealed that three clinical tests accurately predicted post CPR poor neurologic outcome: bilateral absence of pupillary reflexes more than 24 hours after a return of spontaneous circulation, bilateral absence of corneal reflexes more than 24 hours, and bilateral absence of somatosensory-evoked potentials between days 1 and 7. The specificity of these tests further improved when they were performed beyond 72 hours. Data on neuroimaging, biomarkers, or combination testing were considered inconclusive (25).
Quantitative whole-brain white matter fractional anisotropy measured by diffusion tensor magnetic resonance imaging can accurately predict neurologic outcome at 6 months in patients who are unconscious 7 days after cardiac arrest (81).
COVID-19 adversely affected survival rates in patients who received cardiopulmonary resuscitation after in-hospital cardiac arrest, and these patients had low survival rates. Murphy and colleagues reviewed the data of 103 patients with COVID-19 who were resuscitated after in-hospital cardiac arrest (51). Among these 103 patients, 35 (34.0%) had return of spontaneous circulation for at least 20 minutes; however, only 15 (14.6%) patients survived to 30 days. Preceding acute respiratory insufficiency was considered responsible for COVID-19-associated in-hospital cardiac arrest (51).
Artificial intelligence for prediction of prognosis. Systematic reviews investigated the most effective machine learning models for predicting neurologic outcomes after cardiac arrest, focusing on EEG-based models. Analyzing medical and engineering literature, the review identified Random Forest and Convolutional Neural Network as the most common and effective models in conventional machine learning and Deep Neural Network categories, respectively. Random Forest models showed an Area Under AUC range of 0.8 to 0.97, whereas CNN models ranged from 0.7 to 0.92. The most frequent EEG features used were band power, Shannon entropy, and burst-suppression ratio. The findings suggest that combining EEG features with electronic health record data could enhance prognostic accuracy (14; 38).
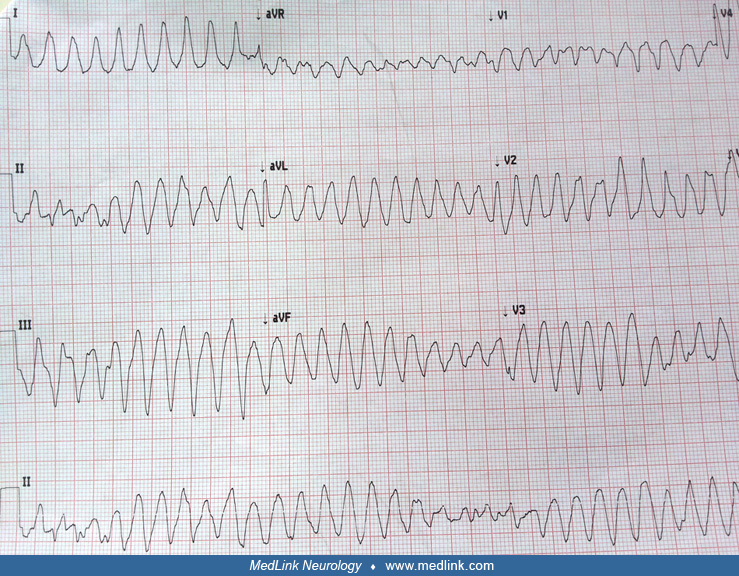
In cardiac arrest, heart activity ceases and circulation stops. Cardiac arrest occurs because of several reasons, such as asystole, pulseless electrical activity, ventricular fibrillation, or pulseless ventricular tachycardia.
Cardiac disorders, like coronary artery disease, cardiomyopathies, cardiac arrhythmias, congenital heart diseases, and valvular heart diseases often predispose a cardiac arrest. The most frequent underlying heart condition predisposing to a cardiac arrest is coronary artery disease. Cardiac arrest may be the first manifestation of coronary artery disease. Risk factors of coronary artery disease (old age, male sex, smoking, hypertension, diabetes mellitus, hypercholesterolemia, obesity, and a family history of coronary artery disease) also predispose for a cardiac arrest. Presence of a left ventricular dysfunction (ejection fraction less than 30% to 35%) is an important risk factor for sudden death (19). Conduction abnormalities that can cause ventricular tachycardia or ventricular fibrillation, like long QT syndrome, Brugada syndrome, and Wolff-Parkinson-White syndrome, can be associated with sudden cardiac arrest. Non-coronary causes, like pulmonary embolism and aortic dissection or aneurysmal rupture, can also cause cardiac arrest. Most patients with in-hospital cardiac arrest has associated systemic disorders, such as myocardial infarction, heart failure, respiratory insufficiency, renal insufficiency, diabetes mellitus, malignancy, and septicemia as well as the need for use of mechanical ventilation and intravenous vasopressors (23).
Post-cardiac arrest syndrome is a distinct pathophysiological entity that appears after successful cardiopulmonary resuscitation. Following a cardiac arrest, whole-body ischemia causes initial diffuse tissue and organ injury. Further damage occurs after systemic blood circulation is restored.
Cardiac arrest leads to a diffuse ischemic injury to the brain. During CPR there is a state of global cerebral hypoperfusion. After return of spontaneous circulation, brain perfusion is restored to normal. The brain requires uninterrupted oxygen supply to sustain normal neuronal function. ATP production ceases within seconds, which leads to rapid dysfunction of ATP-dependent sodium-potassium pumps on the neuronal membrane and acute cerebral dysfunction. This process leads to disruption of the blood-brain barrier, intracellular acidosis, and neuronal edema. Vulnerable structures of the brain, the hippocampus, cortex, cerebellum, corpus striatum, and thalamus are more preferentially affected. In the early post-resuscitation phase, there is increased production of free oxygen radicals and many mediators of inflammation leading to secondary brain injury. When blood spontaneous circulation is restored cerebrovascular autoregulation is impaired, resulting in a varying amount of cerebral edema. Autoregulation failure results in hypoperfusion of some of brain areas. All of these changes lead to further damage to the brain in the post-cardiac arrest phase (53; 12). High-resolution T1-weighted images in 126 anoxic coma patients (16 ± 8 days after cardiac arrest) and 70 matched controls revealed significantly extensive cortical and subcortical brain volumes atrophy. The anatomical regions that were more significantly affected included frontal cortex, posterior cingulate cortex, thalamus, putamen, pallidum, caudate, hippocampus, and brain stem (74). Magnetic resonance spectroscopy (MRS) was performed in 50 patients who had experienced cardiac arrest (39). Fourteen of these patients achieved coma recovery before hospital discharge and were able to obey the commands. MRS in patients who could not recover demonstrated a decrease in total N-acetyl-aspartate (NAA/Cr) and an increase in lactate (Lac/Cr). MRS changes were most prominent in the posterior cingulate gyrus (39).
Post-cardiac arrest myocardial dysfunction does happen in some patients and significantly hampers the recovery following a cardiac arrest. Immediately after spontaneous circulation is restored, a state of diffuse myocardial hypokinesis may appear to lead to extreme variability in heart rate and blood pressure. Acute coronary syndrome may also be responsible for cardiac dysfunction in the post-cardiac arrest phase. Cellular damage after reperfusion of previously viable ischemic tissues is known as “reperfusion injury.” The mechanisms responsible for reperfusion injury are increased production free oxygen radicals, complement system activation, leucocyte-endothelial cell adhesion, platelet-leucocyte aggregation, increased microvascular permeability, and decreased endothelium-dependent relaxation. All these cellular changes may ultimately lead to a state of multiorgan failure (18).
According to the American Heart Association’s “Heart Disease and Stroke Statistics--2014 Update,” 359,400 incidences of out-of-hospital cardiac arrest were recorded in 2013; approximately 40% received CPR, and 9.5% survived following a cardiopulmonary resuscitation. During this period, 209,000 incidences of in-hospital cardiac arrest were recorded. Among these, 23% of adults and 40% of children survived following a cardiopulmonary resuscitation (24). The risk of sudden cardiac death approximately doubles during physical activity and is 2- to 3-fold higher in athletes compared to nonathletes. In the young (younger than 35 years), cardiac arrest is mainly due to congenital or inherited cardiac diseases, whilst coronary artery disease is the most common cause in older athletes (70).
Out-of-hospital cardiac arrest incidence and outcomes vary greatly worldwide. A review including sixty-seven studies from Europe, North America, Asia, and Australia, revealed that the incidence of treated out-of-hospital cardiac arrests was higher in North America (54.6%) than in Europe (35.0%), Asia (28.3%), and Australia (44.0%). In Asia, the percentages of ventricular fibrillation and survival to discharge rates were lower (11% and 2%, respectively) than those in Europe (35% and 9%, respectively), North America (28% and 6%, respectively), or Australia (40% and 11%, respectively) (06).
In a Danish study assessing individuals aged 18 to 85 from 2001 to 2019, researchers found that people with HIV (PWH) have a significantly higher incidence of out-of-hospital cardiac arrest compared to those without HIV (20). Specifically, the incidence in people with HIV was 149 per 100,000 person-years, whereas it was 64 per 100,000 in the general population. People with HIV also tended to experience out-of-hospital cardiac arrest at a younger age. Despite these disparities, the 30-day mortality rates post-out-of-hospital cardiac arrest were similar in both groups. This study highlights HIV as an independent risk factor for out-of-hospital cardiac arrest, underscoring the need for further research to reduce out-of-hospital cardiac arrest occurrences in people with HIV.
The most common underlying condition predisposing to cardiac arrest is coronary artery disease. Cardiac arrest may be the first manifestation of coronary artery disease. Risk factor (eg, age, male sex, cigarette smoking, hypertension, diabetes mellitus, hypercholesterolemia, obesity, and a family history of coronary artery disease) modification is crucial in reducing the risks of coronary heart disease-related death and all-cause mortality. Drugs that were found effective in reducing the risk of cardiac arrest in patients with coronary disease or cardiomyopathy include beta-blockers, angiotensin-converting enzyme inhibitors, and statins (19). The implantation of a cardiac defibrillator is indicated as a secondary prevention strategy for cardiac arrest in patients surviving a life-threatening ventricular arrhythmia that had no reversible or treatable cause. Even patients with left ventricular ejection fraction of 35% or less require implantable cardioverter defibrillator. Secondary prevention is defined as clinical measures in patients who have survived a prior cardiac arrest or sustained ventricular tachycardia (19).
According to the advanced life support guidelines provided by the Resuscitation Council in the United Kingdom, potential causes or aggravating factors for which specific treatment exists must be sought during any cardiac arrest. The Resuscitation Council UK suggested a 4Hs and 4Ts formula for remembering the differential diagnosis of cardiac arrest (The Resuscitation Council UK 2014).
|
4Hs |
|
4Ts |
|
|
Several investigative methods, like electroencephalography, somatosensory-evoked potentials, biomarker estimations, and neuroimaging, may help in determining the prognosis following a cardiac arrest.
During a cardiac arrest, basic CPR by bystanders and early defibrillation is mainstay of treatment in out-of-hospital setting.
Cardiopulmonary resuscitation. CPR consists of mouth-to-mouth respiration (rescue breathing) and chest compression. Chest compression-only CPR is now frequently being used. When a bystander is not trained in CPR, he or she can provide chest compression-only CPR with chest compressions of about 100 per minute. If the bystander is trained in the CPR technique, he or she can perform CPR with 30 chest compressions before giving rescue breaths. A study observed that conventional CPR was more effective and associated with better outcomes than chest compression-only CPR for both 1-month survival and neurologically favorable 1-month survival. The benefit of conventional CPR was significantly better in younger people in noncardiac cases and with a delay in start of CPR after the event was witnessed in noncardiac cases (58). In patients with out-of-hospital cardiac arrest, shorter duration of CPR is associated with likelihood of favorable outcome at hospital discharge (67).
Mechanical chest compression devices are now considered a satisfactory alternative to manual compressions and produce high-quality chest compressions. Preliminary data suggest that mechanical chest compression devices might be superior to conventional manual chest compressions during cardiac arrest. Wang and Brooks reviewed this aspect and suggested that though mechanical chest compression devices are a reasonable alternative, they are associated with higher frequency of chest injury, particularly rib fractures (82). They concluded that mechanical chest compression devices should be reserved for a situation where manual chest compressions are impractical, impossible, or unsafe.
Bystander and first responder resuscitation are crucial for the success of cardiopulmonary resuscitation efforts. Bystander-initiated cardiopulmonary resuscitation is associated with a greater likelihood of survival with favorable neurologic outcome. A study assessed the proportion of bystander and first responder resuscitation efforts, including the combination of efforts between bystanders and first responders, from 2010 through 2013 (45). The combination of bystander cardiopulmonary resuscitation and first responder defibrillation increased from 14.1% in 2010 to 23.1% in 2013. Survival with favorable neurologic outcomes also significantly increased from 7.1% in 2010 to 9.7% in 2013. Approximately 77% of cardiac arrest survivors return to work. Factors associated with return to work (6 or more months of sustainable employment) are male sex, early age, bystander-witnessed arrest, and bystander cardiopulmonary resuscitation (34). Prehospital resuscitation efforts should be done for at least 40 minutes in bystander-witnessed out-of-hospital cardiac arrest (52).
In a multicenter, randomized trial in the Netherlands comparing extracorporeal CPR with conventional CPR in patients with refractory out-of-hospital cardiac arrest, 160 patients were initially enrolled (78). After exclusions, 70 received extracorporeal CPR and 64 conventional CPR. The primary outcome was survival with favorable neurologic function at 30 days. Results showed 20% in the extracorporeal-CPR group and 16% in the conventional-CPR group achieved this outcome, with no significant difference between the two (odds ratio 1.4, P = 0.52). The incidence of serious adverse events was similar in both groups, indicating comparable effectiveness of both CPR methods in these patients (78).
Oxygenation and ventilation. Basic airway management is crucial. Proper ventilation can be assured by manually relieving any upper airway obstruction and by providing bag-valve mask ventilation or the insertion of an oropharyngeal or nasopharyngeal airway. Endotracheal intubation or bag-mask ventilation is often used for prehospital airway management in patients with cardiac arrest. The choice of airway management technique in out-of-hospital cardiac arrest has always been controversial. In one study, bag-valve-mask ventilation was found better in comparison with the advanced airway management systems that also included use of supraglottic airways. Of 649,359 patients with out-of-hospital cardiac arrest, 367,837 (57%) underwent bag-valve-mask ventilation and 281,522 (43%) advanced airway management, including 41,972 (6%) with endotracheal intubation and 239,550 (37%) with use of supraglottic airways. In the full cohort, the advanced airway group experienced a lower rate of favorable neurologic outcomes as compared with the bag-valve-mask group (1.1% vs. 2.9%). Neurologically favorable survival was significantly lower both for endotracheal intubation and for use of supraglottic airways (27).
Defibrillation. Defibrillation is a process that helps in restoring a normal rhythm to the heart. Small portable defibrillators, called automated external defibrillators, have become widely available. A prospective study in Japan suggested that early defibrillation, irrespective of defibrillation being done by a bystander or emergency medical service personnel, was significantly associated with neurologically favorable outcomes. The study included consecutive out‐of‐hospital cardiac arrest patients with resuscitation attempts over a period of 7 years (2005 to 2011). A total of 9,453 bystander‐witnessed, out‐of‐hospital cardiac arrests of cardiac origin were documented, and 894 (9.5%) of them occurred in public places. Mean time from collapse to shock was 5.0 minutes among those who received shocks with public‐access defibrillation devices. Automated external defibrillators were delivered to over 40% of bystander‐witnessed, out‐of‐hospital cardiac arrests, and time to shock was shortened (50).
Prehospital epinephrine administration. Epinephrine use during cardiac arrest may not be associated with improved survival to hospital discharge (60). Patients receiving prehospital adrenaline were 2.89 times more likely to achieve prehospital return of spontaneous circulation than those not administered adrenaline. However, there were no significant effects on overall return of spontaneous circulation, admission, and survival to discharge (02). Similar findings were noted in a Japanese study as well. Among patients with out-of-hospital cardiac arrest in Japan, use of prehospital epinephrine was significantly associated with increased chance of return of spontaneous circulation before hospital arrival. However, there was a decreased chance of survival and good functional outcomes 1 month after (26). A randomized controlled study observed that in adults with out-of-hospital cardiac arrest, the use of epinephrine resulted in a significantly higher rate of 30-day survival (63). However, no significant difference was noted in favorable neurologic outcome. Epinephrine hydrochloride has potent alpha-adrenergic receptor-stimulating effects. Initially, 1 mg epinephrine is given by intravenous administration. Epinephrine 1 mg may be repeated every 3 to 5 minutes. A systematic review and metaanalysis comprising of data from 17 trials (21,510 patients) suggested that a standard dose of epinephrine improves survival but not neurologic outcomes in out-of-hospital cardiac arrest patients (03).
The results of double-blind, randomized placebo-controlled trial (PARAMEDIC-2) have raised some concerns that epinephrine leads to increased numbers of survivors with damaged brain (63; 75). In fact, epinephrine has more pronounced effects for nonshockable rhythms when given early, and it increases the number of survivors all kinds including those having brain damage.
Post-resuscitation management. Post-resuscitation management is also crucial for better prognosis. Patients with cardiac arrest in post-resuscitation phase often require intubation and a need for mechanical ventilation for a period of time. Patients with evidence of coronary artery disease (ST-elevation myocardial infarction) should be managed regardless of coma or induced hypothermia. Immediate angiography and percutaneous coronary intervention may be needed in survivors with ST-segment elevation myocardial infarction. Vasoactive drugs may be administered after post-resuscitation phase to support cardiac output. The post-cardiac arrest patient is likely to develop metabolic abnormalities, such as hyperglycemia, which may be detrimental and must be aggressively managed (61). Use of antiarrhythmic drugs like amiodarone or lidocaine do not result in a significantly higher rate of survival or favorable neurologic outcome among patients with out-of-hospital cardiac arrest due to initial shock-refractory ventricular fibrillation or pulseless ventricular tachycardia (36). Sodium bicarbonate administration in out-of-hospital cardiac arrest is frequently administered with the purpose to counteract acidosis. However, there is limited clinical evidence to support this practice. In a retrospective study involving the review of 23,567 records, 6,663 (28.3% of which received sodium bicarbonate) indicated that sodium bicarbonate administration was associated with better survival in adult cardiac arrests with nonshockable rhythms and asystole (54). In pediatric cardiac arrests, sodium bicarbonate administration was associated with lower rates of survival to hospital discharge (11).
Coronary angiography and angioplasty. Chances of favorable neurologic recovery are higher following immediate coronary angiography, with or without percutaneous coronary angioplasty, in a resuscitated out-of-hospital cardiac arrest patient. Early coronary reperfusion possibly improves the chances of survival (28; 30).
Therapeutic hypothermia. Therapeutic hypothermia possibly increases the survival and neurologic recovery following a cardiac arrest. Therapeutic hypothermia protects nerve cells by reducing the production of damaging free oxygen radicals and inflammatory changes, which are possible mechanisms of neuronal injury after a period of ischemia. All unconscious patients should be cooled to 32° to 34° C for 12 to 24 hours. Targeted body temperature has always been a controversial issue. A randomized trial was conducted in comatose survivors of out-of-hospital cardiac arrest with the objective of comparing the efficacy of moderate hypothermia (31 °C) versus mild hypothermia (34 °C) on clinical outcomes in comatose survivors (40). The authors failed to establish the superiority of moderate hypothermia (31 °C) in reducing deaths or poor neurologic recovery. In a randomized trial, Dankiewicz and colleagues noted that targeted hypothermia at 33°C did not produce better outcomes than targeted normothermia with early treatment of fever (body temperature 37.8°C or higher) (15). Moreover, 6-month mortality or disability was not different between the groups. A metaanalysis aimed to determine if hypothermia at 33°C enhances survival and functional recovery compared to controlled normothermia in unconscious adults resuscitated from out-of-hospital cardiac arrest with an initial nonshockable rhythm (79). It involved a metaanalysis of two multicenter, randomized clinical trials with blinded outcome assessors. The study included unconscious out-of-hospital cardiac arrest patients with a nonshockable initial rhythm. Participants were randomly assigned to either a hypothermia treatment at 33°C or a normothermia treatment within the range of 36.5 to 37.7 °C for a minimum of 24 hours. The analysis considered various factors, such as age, sex, initial rhythm, and time to return of spontaneous circulation. The primary outcome measured was mortality at 3 months, and the secondary outcome was unfavorable functional outcome, defined by a Cerebral Performance Category score of 3 to 5. The study included a total of 912 patients, with a fairly even split between the hypothermia and normothermia groups. The results showed that at 3 months, 80.1% in the hypothermia group and 82.1% in the normothermia group had died, indicating no significant difference in survival. Similarly, the functional outcomes were comparable between the two groups. The conclusion of this metaanalysis was that hypothermia at 33°C for unconscious survivors from out-of-hospital cardiac arrest with an initial nonshockable rhythm did not significantly improve survival or functional outcome compared to controlled normothermia (79).
A cooling device, such as cooling pads, cooling blankets, and ice packs, is used to reduce the patient’s core body temperature. Temperature is monitored using a bladder temperature probe (72). An investigation revealed that among comatose survivors of out-of-hospital cardiac arrest, inhaled xenon combined with hypothermia compared with hypothermia alone resulted in less white matter damage (37). White matter damage was measured by using fractional anisotropy of diffusion tensor MRI. However, reduction in white matter damage did not affect neurologic outcomes or mortality at 6 months. An American Academy of Neurology guideline noted that for patients who are comatose and have an initial cardiac rhythm of either pulseless ventricular tachycardia or ventricular fibrillation, therapeutic hypothermia is highly likely to be effective in improving functional neurologic outcome and survival (22).
In comatose children survivors of out-of-hospital cardiac arrest, therapeutic hypothermia was not found beneficial with a good functional outcome at 1 year. A study showed that there was no significant difference in the primary outcome between the hypothermia group and the normothermia group (20% vs. 12%) (49).
Hypercapnia. In a study involving 1700 patients resuscitated after out-of-hospital cardiac arrest and admitted to the ICU, researchers compared the effects of mild hypercapnia (targeted partial pressure of arterial carbon dioxide [Paco2] of 50 to 55 mm Hg) with normocapnia (Paco2 of 35 to 45 mm Hg) on neurologic outcomes (16). The primary goal was to assess favorable neurologic outcomes using the Glasgow Outcome Scale-Extended at 6 months. The study found no significant difference in favorable neurologic outcomes or 6-month mortality rates between the mild hypercapnia and normocapnia groups. This suggests that targeted mild hypercapnia does not improve neurologic outcomes compared to normocapnia in these patients.
Extracorporeal membrane oxygenation. Extracorporeal membrane oxygenation system is employed for cardiopulmonary resuscitation in nonresponsive patients to conventional cardiopulmonary resuscitation. Data suggest that the extracorporeal membrane oxygenation system is associated with high rates of neurologic morbidity and mortality. Younger patients are likely to have better neurologic function after discharge from the hospital (04).
An exploratory analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) trial focused on the effects of targeted hypothermia versus normothermia on functional outcomes, particularly societal participation and cognitive function in survivors 6 months after OHCA (41). The study, encompassing 1861 comatose adult patients, found no significant difference between the two interventions in terms of societal participation (measured by the Glasgow Outcome Scale Extended) or cognitive function (assessed by the Montreal Cognitive Assessment and the Symbol Digit Modalities Test). Many survivors still faced limitations in societal participation and mild cognitive dysfunction 6 months post-arrest.
Approximately 1 in 12,000 hospitalizations for delivery is complicated by cardiac arrest, most frequently due to hemorrhage, heart failure, amniotic fluid embolism, or sepsis. Among patients with cardiac arrest, 59% of patients survived to hospital discharge (48). The latest Society for Obstetric Anesthesia and Perinatology consensus statement on the management of cardiac arrest in pregnancy suggested key elements for cardiac arrest in pregnancy. High-quality chest compressions should be immediately started. Left uterine displacement is recommended if the uterus is palpable or visible. Defibrillation should be performed for shockable rhythms as soon as possible. Oral airways are preferred over nasal airways in pregnant patients for airway management and ventilation. Intravenous access should be gained as quickly as possible. Epinephrine and other resuscitation drugs may be used according to need. These guidelines recommend rapid delivery of the fetus in unresponsive maternal cardiac arrest. After spontaneous circulation is restored in an undelivered patient, left uterine displacement should be maintained to optimize uterine blood flow. Therapeutic hypothermia may be considered for postpartum patients of cardiac arrest (43).
So far, the ongoing COVID-19 epidemic has led to 2,684,093 deaths. The COVID-19 epidemic has had a major impact on the epidemiology, diagnosis, management, and outcome of cardiac arrest. Early reports indicated that during the COVID-19 pandemic, the incidence of out-of-hospital cardiac arrest increased by 58%, but bystander cardiopulmonary resuscitation decreased by 15.6% (64). Chance of survival in cases of out-of-hospital cardiac arrest was poor. Even increases in the number of in-hospital cardiac arrests were noted. Patients with in-hospital cardiac arrest had better chance of survival (85).
Sultanian and colleagues evaluated the outcome among cardiac arrest cases with COVID-19 (77). The authors enrolled all the patients recorded in the Swedish Registry for Cardiopulmonary Resuscitation from January 1, 2020 to July 20, 2020. They analyzed 1946 cases of out-of-hospital cardiac arrest and 1080 cases of in-hospital cardiac arrest. Among these, 88 (10%) of out-of-hospital cardiac arrests and 72 (16%) of in-hospital cardiac arrests had SARS-COV-2 infection. Authors noted 3.4 times increased 30-day mortality in COVID-19-positive cases, compared with COVID-19-negative cases. COVID-19 adversely affected the 30-day survival, which was 4.7% COVID-19 positive patients, 9.8% for patients without COVID-19, and 7.6% in the pre-pandemic period. Analysis of in-hospital cardiac arrest data revealed that the odds ratio for COVID-19-positive cases versus COVID-19-negative cases was 2.27. The 30-day survival after in-hospital cardiac arrest was 23% in COVID-19-positive patients, 39.5% for patients without COVID-19, and 36.4% in the pre-pandemic period (77). A metaanalysis analyzed the impact of the COVID-19 pandemic on out-of-hospital cardiac arrest incidence, bystander CPR rates, and patient outcomes. A meta-analysis of individual patient data from 10 studies showed increased out-of-hospital cardiac arrest incidence, especially in regions with the highest weekly COVID-19 rates (> 136 per 100,000 inhabitants). There was a notable decrease in bystander CPR in these high-incidence areas. The pandemic period also saw more out-of-hospital cardiac arrests with medical etiology and at home, along with a decrease in shockable initial rhythms. Importantly, the COVID-19 period was linked to higher pre-hospital death rates and lower survival to hospital admission and discharge, regardless of regional COVID-19 incidence (05).
A systematic review evaluated the incidence, characteristics, and outcomes of in-hospital cardiac arrest in COVID-19-affected patients (42). This review included data of 847 in-hospital cardiac arrests from eight studies. Incidence of in-hospital cardiac arrest was 1.5% to 5.8% among hospitalized patients, whereas incidence was 8% to 11.4% among patients in intensive care units. In the majority, initial heart rhythms were nonshockable (asystole or pulseless electrical activity). There were lesser deaths in intensive care unit settings (88.7% vs. 98.1%). Patients 60 years of age or above had higher in-hospital mortality (42).
Hayek and colleagues analyzed the data of in-hospital cardiac arrest among 5019 critically ill patients with COVID-19 (29). The authors noted that 14% (701 out of 5019) of critically ill patients had in-hospital cardiac arrest. Out of these, 57% (400 out of 701) received cardiopulmonary resuscitation. Old age, comorbidities, and admission in small hospitals predicted the risk of cardiac arrest. The most common rhythms encountered were pulseless electrical activity and asystole. Forty-eight (12%) of the 400 patients who received cardiopulmonary resuscitation survived. Only 7% (28 out of 400) of cardiopulmonary resuscitation survivors had normal or mildly impaired neurologic status at discharge.
Certain precautions are recommended while performing cardiopulmonary resuscitation on COVID-19-affected patients. The face of an individual with cardiac arrest needs to be covered by the cloth, so as to minimize the dispersion of respiratory droplets. The rescuer should also cover his/her face. Rescue breaths need to be avoided. Chest compression should be done at the rate of 100 to 120 compressions per minute. An automated external defibrillator should be used as soon as possible (64).
Anesthesia-related cardiac arrests are rather infrequent. In one survey, 160 perioperative cardiac arrests within 24 hours of surgery were identified from an anesthesia database of 217,365 anesthetics (17). In this survey, 14 cardiac arrests were attributed to anesthesia. In 23 cardiac arrests, anesthesia possibly contributed to the event. Cardiac arrests were caused by airway complications that occurred primarily with induction or emergence or in the post-anesthesia care unit. Anesthesia‐related cardiac arrest often has a favorable outcome. In another survey involving a pediatric population, 193 arrests (49%) were related to anesthesia. Cardiovascular disorders, hypovolemia from blood loss, and hyperkalemia from transfusion of stored blood are the most common identifiable circulatory causes of cardiac arrest in perioperative set up. Among respiratory causes of arrest, airway obstruction from laryngospasm was the most common cause. Vascular injury incurring during placement of central venous catheters was the most common equipment-related cause of arrest. Cardiac arrest occurred most commonly in the surgical and postsurgical phases (08). In the registry of 40,271 cases of spinal anesthesia in Thailand, 11 cardiac arrests were recorded with a mortality of 90.9%. In four patients, the anesthetic contributed directly to the arrest, like high sympathetectomy, local anesthetic overdose, or lack of electrocardiography monitoring, whereas some arrests were associated with specific events, like cementing of the prosthesis, massive bleeding, suspected pulmonary embolism, and suspected myocardial infarction (13).
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Ravindra Kumar Garg DM
Dr. Garg of King George's Medical University in Lucknow, India, has no relevant financial relationships to disclose.
See Profile
Matthew Lorincz MD PhD
Dr. Lorincz of the University of Michigan has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
General Neurology
Jan. 13, 2025
General Neurology
Jan. 13, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 08, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 07, 2025
General Neurology
Dec. 30, 2024
General Neurology
Dec. 13, 2024
General Neurology
Dec. 13, 2024
Neuromuscular Disorders
Dec. 09, 2024