General Neurology
Neurologic manifestations of celiac disease and gluten sensitivity
Jan. 23, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Stereotactic neurosurgery is a rapidly growing aspect of treatment for nervous system disorders. It typically involves the use of advanced imaging techniques (CT, MRI) and devices to translate the imaging information into guidance for the neurosurgical procedure. Stereotactic neurosurgery has progressed from the use of a cumbersome frame placed on the patient’s head under anesthesia for simple probe (eg, biopsy needle, electrode) localization to a multifaceted set of techniques that can incorporate various anatomic, metabolic, and functional data sets to permit precise interventions on any area of the brain or spinal cord. Neurosurgical robots and augmented reality with head-mounted displays can minimize human error and improve functionality in stereotactic neurosurgery. Future developments will include precisely implanted multifunctional “effectors” (micro- and nano- devices such as electrodes, infusion catheters, and controlled-release capsules) to greatly expand the types of disorders benefiting from stereotactic neurosurgery.
|
• Stereotactic neurosurgery (three-dimensional localization in the nervous system) began with animal research early in the 20th century; procedures in humans began in the middle of the 20th century. | |
|
• Until the 1990s, stereotactic neurosurgery usually involved placing a frame on the patient’s head under local anesthesia. | |
|
• Frameless stereotactic neurosurgery registers points on the patient’s face, skull, or spine with imaging (CT or MRI scan) to allow precise localization of the desired target in the central nervous system. | |
|
• Major applications of stereotactic neurosurgery include stereotactic radiosurgery (over the past 45 years) and deep brain stimulation (over the past 30 years). | |
|
• The integration of stereotactic neurosurgery with robots is at present the most rapidly developing aspect of the field, resulting in more precise and minimally invasive neurosurgical procedures involving the brain and spine. |
Early in the 20th century, Horsley and Clarke devised a stereotaxic system for studying neurophysiology (21). Mussen devised the first stereotactic frame intended for human use in 1918. Although the frame was never used, Mussen presciently described minimally invasive stereotactic surgery for the diagnosis and treatment of brain tumors (39). In a 1971 letter to his son, an engineer, Mussen wrote,
|
My idea…was to make a complete instrument of the human brain and then make an atlas of the human brain like in the cat. Then you could locate any structure in the human brain by looking at the atlas and it was my thought that if there was a tumor in the brain that could not be located, you could send an electrode in and get the reaction of a normal brain and the difference if you came to the tumor. And then by making a number of degenerations with the galvanic current you might be able to destroy the tumor. And all this could be done through a 5 mm trephine in the skull and puncturing the dura without exposing the brain at all. |
However, it was not until the World War II era that stereotaxic techniques were developed to explore the deep brain nuclei in both animals and humans (45). Following World War II, the Temple University team in the United States and the Talairach team in France continued working on stereotactic frames for use in man. The Temple team was first in publishing their work; the initial stereotactic target was the globus pallidus in patients with Huntington chorea (46; 15).
Initially, stereotaxic neurosurgery relied on a referential system called a "stereotaxic frame.” The frame is attached to the skull and serves to position the necessary instruments.
In 1950 Talairach proposed the bicommissural line of the third ventricle (anterior commissure to posterior commissure), visualized by means of ventriculography, as the zero or reference plane. In 1956 during the First International Congress of Neurology, Talairach and colleagues presented their first stereotactic atlas based on the bicommissural line (53). Stereotactic approaches to spinal lesions were proposed in 1969 (18) and have undergone considerable development (25; 36).
A subset of stereotactic neurosurgery is stereotactic radiosurgery, the use of stereotactic techniques to direct multiple doses of radiation toward a specific target (usually from 2 to 3 mm up to 2 to 3 cm in diameter). Stereotactic radiosurgery is the subject of another article (titled Stereotactic radiosurgery) and will not be discussed here.
Regarding nomenclature, the technique was initially called "stereotaxic,” but during the 1970s the term "stereotactic” came into use. The terms have since been differentiated: "stereotaxic" when used in animals and "stereotactic" when used in humans. “Stereotaxy" is applied to both (14).
A compendium of stereotactic neurosurgery has been edited by three of the most significant contributors to the field (29). The role of psychosurgery in the evolution of stereotactic and functional neurosurgery during the second half of the 20th century has been published (41). A comprehensive, well-illustrated history of stereotactic atlases (a key component of stereotactic neurosurgery) is available (09).
|
• Stereotactic neurosurgery employs a coordinate system (typically three planes at right angles) to localize the desired point in the brain accurately. | |
|
• Preoperative imaging (usually an MRI scan) is used to determine the safest route to the desired point (tumor or other lesion to be excised). | |
|
• Neuro-navigation is a term used where the stereotactic coordinates to not utilize a frame placed on the patient’s head but rather to translate the reference points on the preoperative imaging to intraoperative guidance for the surgeon. | |
|
• Robots are being employed for stereotactic neurosurgery with the future goal of having certain neurosurgical operations completely automated. | |
|
• Holographic visualization using head-mounted displays promises to enhance both preoperative planning and education for stereotactic neurosurgery. |
Acquisition of the stereotactic target is performed prior to surgery using CT, MRI, or digital/CT/MR arteriography, with either fiducials (small markers either adherent to the skin or screwed into the outer table of the skull under local anesthesia) or the stereotactic frame in place. In frame-based stereotaxy, a laptop computer is used to locate cerebral targets in relation to the frame’s fiducials and to calculate trajectories of approaches. In frameless stereotaxy, a computer workstation, an array of tracking cameras, and a video monitor are used to present the target within the 3-D CT and MRI image of the patient’s brain and to track the trajectory of the instruments used to approach the target. An advance allows awake craniotomy to be performed with stereotactic image guidance: the reference array is clamped to the margin of the craniotomy rather than using a ring attached to the patient's skull by pin fixation (05).
The principal types of frame-based stereotactic systems are the arc system and the burr-hole mounted.
A typical frameless stereotactic system, the Stealth, includes the workstation, video monitor, camera array, and surgical instruments. The most recent advances include the “smart” operating room incorporating intraoperative imaging (MRI/PET/CT), multiple ultrasound techniques, laser and other forms of precision tissue ablation, robotic devices such as neuroArm, and workstations for both virtual rehearsals of complex neurosurgical procedures and telesurgery (ie, where the neurosurgeon is remote from the operating room site).
Deep brain stimulation (DBS) involves the use of stereotactic techniques to place one or more electrodes into the brain with high spatial accuracy (a millimeter or less). The electrodes are connected to a pulse generator (microprocessor and battery, similar to a cardiac pacemaker) customarily placed subcutaneously inferior to the clavicle (again, similar to a cardiac pacemaker). The connecting wires or leads run subcutaneously to the entry point(s) in the skull for the electrode(s). The primary indications for deep brain stimulation include movement disorders (eg, Parkinson disease, essential or familial tremor, dystonia), although other indications are being investigated (eg, epilepsy and mood disorders), but so far with less success than with movement disorders. A comprehensive review of stereotactic neurosurgery for mood disorders has been published (57).
Although intraoperative recording of brain electrical activity during electrode placement has been used to increase the odds of success, improvements in neuroimaging have encouraged some centers to rely solely on imaging to guide electrode placement (07). This allows the use of a general anesthetic, which is essential in pediatric or uncooperative patients. Emerging advances in neuroimaging promise increasingly accurate electrode placement without electrophysiological recording. One such neuroimaging advance is diffusion tractography imaging (DTI) to visualize the white matter tracts within the brain (08). DTI uses new MRI protocols to visualize the diffusion of water molecules; because water molecules diffuse parallel to the direction of axons rather than perpendicular, white matter tracts (axons) can be visualized. It has been hypothesized that much of the effect of deep brain stimulation on brain function is due to white matter tract stimulation (31). DTI has reached the point where the accuracy of DTI to map functional circuitry has been compared across different subjects and different MRI manufacturers (22).
The combination of precision stereotactic neurosurgery techniques with advanced neuroimaging techniques promises to improve the efficacy of deep brain stimulation significantly in the coming years. One publication presents evidence that a fully automated image registration technique (using the Food and Drug Administration–approved CranialVault software brain atlas) is superior to techniques relying on either standard stereotactic coordinates or on identifying the target on the patient’s MRI scan (38). The demonstration of holographic visualization using head-mounted displays is likely to significantly improve both the efficacy of preoperative planning for deep brain stimulation surgery and the educational aspects of stereotactic neurosurgery (35). Holography allows the overlaying of various imaging aspects (eg, grey versus white matter, blood vessels, fiber tracts) with various electrode trajectories (and simulated effects of stimulation). Head-mounted displays allow individuals in various locations around the world to share the preoperative planning or educational aspects of holographic visualization in real time (42).
Stereotactic neurosurgery aims to reach, with precision and safety, any point in the brain or spinal cord for diagnosis or therapy by means of minimally invasive tools through a system of interrelated Cartesian or polar anatomical coordinates. In a broader definition, stereotactic neurosurgery includes image guidance and other techniques to treat disorders of the spine such as disc disease and instability. Issues include (1) localization errors due to MRI field inhomogeneities, fiducial registration inaccuracies, and intraoperative brain shift (due to positioning, CSF drainage, or tumor removal) and (2) complications, most notably brain hemorrhage in closed biopsies, ablations, and deep brain stimulation procedures.
Accuracy results from precise detail to fiducial registration as well as the use of fine-cut (usually 1 to 2 mm) CT or MRI scans. Image fusion and the incorporation of MR angiography, functional MRI data, etc. have improved the usefulness and safety of stereotactic neurosurgery. A review of the factors involved in the accuracy of stereotactic neuro-navigation systems has been published (52).
A major advance on the horizon is the incorporation of electrical and chemical information in addition to neuroanatomical information for localization. Nanoprobes that can monitor both electrical activity and neurotransmitter levels (while stimulating the brain both focally and at many locations) will be feasible for clinical use in the near future (02; 03).
Stereotactic neurosurgery has broadened its indications remarkably over the past 30 years. The majority of stereotactic procedures during the 1950s and 1960s were thalamotomies for the treatment of movement disorders (13). With the discovery of l-dopa as an effective treatment for Parkinson disease in 1968, the number of stereotactic procedures performed dropped by more than 90%. A renaissance in stereotactic procedures occurred with the advent of the CT scan: the Leksell stereotactic frame was adapted to CT scan localization, and stereotactic frames were developed to utilize CT scan information directly (without regard to positioning of the patient in the CT scanner), most notably the Brown-Roberts-Wells frame (13). There has been an accompanying resurrection of psychosurgery, with stereotactic interventions erasing the stigma of frontal lobotomy (30). Similar procedures have proven useful for some recalcitrant pain patients (56).
The indications for stereotactic neurosurgery fall into several broad categories:
|
(1) An adjunct to open neurosurgical procedures, to place the craniotomy precisely and, thus, minimize the craniotomy size. | |
|
• an electrode for precise lesioning (eg, thalamotomy, pallidotomy) | |
|
(5) Minimally invasive spinal neurosurgery | |
Accurate brain biopsy remains a major goal of stereotactic neurosurgery. An overview of the state-of-the-art in stereotactic brain biopsies surveys the technologies available to improve both diagnostic accuracy and patient safety (06).
The most rapidly expanding indication for stereotactic neurosurgery currently is deep brain stimulation, as described below. Although deep brain stimulation is presently most effective for movement disorders such as Parkinson disease, dystonia, and essential tremor, the largest potential patient population is psychiatry neurosurgery (mood disorders/depression). The parallel development of image-guided techniques for stereotactic neurosurgery and psychiatric neurosurgery is the topic of a review (11; 57). Another rapidly evolving application of stereotactic neurosurgery is the precise implantation of stem cells in the central nervous system, as indicated by a study of human neural stem cells stereotactically implanted in the putamen of patients who had suffered an ischemic stroke (23).
The cost of implanted hardware (tens of thousands of US dollars) and the need for close follow-up make deep brain stimulation impractical for much of the world’s population. Thus, techniques that avoid implants, such as MRI-guided radiofrequency thalamotomy for tremor (both essential tremor and Parkinson disease tremor), remain an important aspect of stereotactic neurosurgery (55).
Because stereotactic neurosurgery can be performed under either local or general anesthesia, there are few contraindications to stereotactic surgery. The two most salient contraindications are the following:
|
(1) The possibility that the target (or the trajectory to the target) is vascular (eg, a vascular malformation or a tumor with hemorrhagic tendencies). Intracranial hemorrhage without the immediate access of an open craniotomy can be fatal. | |
|
(2) Uncorrectable coagulopathy, likewise, is an absolute contraindication to closed stereotactic neurosurgery because of the risk of intracranial hemorrhage. |
Because of the many factors involved in comparing outcomes of stereotactic neurosurgery with nonstereotactic neurosurgery, direct comparison is difficult. In general, once the “team approach” has become natural at a given neurosurgery center, the extra time required for stereotactic techniques (eg, preoperative or intraoperative CT or MRI) is more than offset by shorter time in actual surgery (smaller incisions, fewer returns to surgery for incomplete tumor resections, etc.). Additionally, postoperative hospitalization can be greatly reduced by the minimally invasive techniques (with concomitant decrease in overall cost). The benefits of stereotactic intracranial hemorrhage evacuation (in terms of both patient outcome and total health care expenses) have been documented in a large, randomized study involving 121 surgical patients (17). It is not uncommon for an otherwise healthy patient undergoing stereotactic, image-guided craniotomy for brain tumor to be discharged within 12 hours of surgery; the vast majority of stable patients are discharged within 72 hours of surgery.
The major risk of stereotactic neurosurgery is in closed procedures where intracranial hemorrhage can result in major permanent neurologic deficit or death. Thus, patients with any coagulopathy, those who may harbor a vascular lesion, or those whose intracranial target requires traversing an intracranial blood vessel or vascular region such as the ventricular choroid plexus or ependyma are excluded from closed stereotactic biopsy.
Definitive data are not available regarding improved prognosis in patients undergoing stereotactic versus nonstereotactic procedures, but decreased morbidity and fewer re-operations in procedures such as ventricular shunt catheter placement and brain tumor resections suggest that stereotactic techniques improve prognosis substantially.
The risk of a CT or MRI scan during pregnancy must be included in the risk of a stereotactic procedure. However, a reduction in actual surgery time can result from minimally invasive stereotactic techniques, particularly if the procedure can be performed under local anesthesia or intravenous sedation rather than general anesthesia with its attendant risks to the fetus.
The following two clinical examples illustrate differing applications of stereotactic techniques:
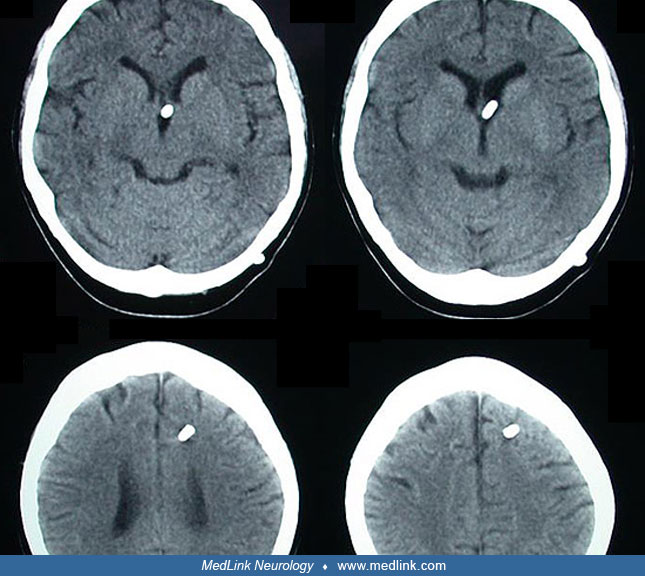
(1) The patient was a 5-year-old male, who presented with headache, vomiting, and ataxia. The upper series of images displayed the intact tumor (pilocytic astrocytoma) prior to surgery. The lower images, taken intraoperatively, defined a residual nubbin of the tumor, cryptic to the surgeon, despite the use of the operating microscope. This remaining tumor, which was detected by intraoperative MRI, was then excised, preventing the need for reoperation.
(2) The patient was a 39-year-old female with a history of progressively worsening headaches over many years plus tonic-clonic seizures not fully controlled by antiepileptic medications. CT and MRI scans showed a suprasellar/3rd ventricle cyst (without evidence of tumor or nidus) and associated obstructive hydrocephalus of the lateral ventricles. Image-guided placement of a ventricular catheter that extended into the cyst as well as the lateral ventricle (ie, cystoventriculoperitoneal shunt) allowed a minimally invasive treatment for both the cyst and the hydrocephalus, as demonstrated on CT scan 6 months postoperatively.)
The principle underlying stereotactic localization was initially conventional radiology: anterior-posterior and lateral radiographs. Stereotactic angiography was added to increase accuracy and reproducibility. Detailed anatomical atlases (53; 43) have appeared in electronic, interactive versions (37; 54).
With the advent of CT in the mid-1970s followed by MRI in the mid-1980s, coordinate systems for stereotactic localization were developed that relied on fiducials and their spatial relationship with the target. These systems initially utilized a frame fixed to the skull (using pins, placed under local anesthesia, into the outer table of the skull, or to a burr hole in the skull), which remained on the patient's head through the preoperative CT or MRI scan until the completion of the procedure. The frame, although accurate to 1 to 2 mm, is cumbersome for the surgeon and inconvenient for the patient.
Frameless stereotactic devices appeared in the early 1990s. Similar to a global positioning system, or GPS, the surgical instruments are tracked by a camera system or by encoders on the joints of a stereotactic arm.
Either temporary skin markers or anatomical landmarks on the patient's head serve as fiducials. In essence, the surgeon is able to track the position of the surgical instruments on a 3-dimensional rendering of the brain (a video monitor presenting the brain MRI or CT) in real time during surgery. The reduction in actual surgery time and shortened postoperative hospital stay because of a smaller cranial incision and less brain trauma more than offset the modest increase in preoperative time spent in scanning with fiducials and preoperative setup. MR arteriography, MR spectroscopy, functional MRI, magnetoencephalography, and other advanced techniques are being used to improve the efficacy of image-guided stereotactic neurosurgery (44).
Although frameless stereotaxy and image-guided techniques have been major advances in neurosurgery, they rely on archived (preoperative) images and, therefore, are unable to account for the inevitable brain shifts that accompany cranial neurosurgery. Entraining CT or MRI devices into the operating room permits both updating target localization and confirms target penetration by the stereotactic biopsy needle and detection of complications such as hemorrhage prior to leaving the operating room. This concept was pioneered at Harvard University, where researchers developed a fixed (floor-mounted), 0.5 T “double doughnut” system with General Electric Medical Systems (01). The surgeon operates within the constraints of the machine, and all tools, including high-speed drills and microscopes, are custom-built from MR-compatible materials. To minimize the impact of intraoperative imaging on patient positioning and access, the University of Calgary and the National Research Council of Canada have designed a ceiling-mounted (mobile)1.5 T magnet (51).
This device permits unfettered access to the cranium, normal positioning, and the benefits of increased signal-to-noise ratio images. A preoperative surgical planning image is obtained, followed by intermittent intraoperative images to confirm the accomplishment of surgical objectives. The head is draped for the acquisition of these images, and the microscope moved beyond the 5 Gauss line.
The latest iteration of the image-guided neurosurgical operating room is exemplified by AMIGO (Advanced Multimodality Image Guided Operating suite) at the Brigham and Women’s Hospital and Harvard Medical School.
AMIGO incorporates a ceiling-mounted 3T MRI (similar to the system developed at the University of Calgary) with a PET/CT scanner for improved tissue identification and localization, most notably for tumor surgery but also – in the near future – for functional neurosurgery. The MRI/PET/CT imaging is combined with a stereotactic navigation system, operating microscope, various ultrasound techniques, laser, and other methods for identifying tissues (eg, tumors) and sampling or ablating those tissues as indicated.
Stereotactic techniques have been combined with robots to enhance the precision of neurosurgical procedures. The first robot designed specifically for neurosurgery was NeuroMate. This robot was initially developed in France for procedures such as brain biopsy and the placement of deep brain electrodes. An iteration of robotically assisted neurosurgery is the ROSA stereotactic robot, also developed in France. The ROSA has been used to compare the accuracy of frameless preoperative MRI imaging, frame-based preoperative CT imaging, and frameless intraoperative CT imaging (the Medtronic “O-Arm” intraoperative CT) (27). The findings were consistent with the literature in that frame-based imaging is modestly (perhaps clinically significantly) more accurate than frameless imaging.
Robotically assisted stereotactic neurosurgery is likely to be as accurate, and possibly more accurate, than nonrobotic techniques (34; 19). Although yet to gain widespread acceptance as "neurosurgical robots," the increasing acceptance of surgeon-guided robots such as the DaVinci suggests that the ability to overcome handicaps such as physiologic tremor and human error will result in widespread use of neurosurgical robots in the future. The interested reader is directed to a review of robots for stereotactic neurosurgery (12).
To capitalize on the benefits of intraoperative MRI guidance, an ambidextrous, MRI-compatible robot (“neuroArm”) has been designed by the University of Calgary and MacDonald Dettwiler and Associates in Ontario (28). The neuroArm robot has been integrated with a virtual reality display similar to the DaVinci surgical robot, which allows the neurosurgeon – potentially at a site remote from the operating room – to perform a procedure with all the information provided by a “smart” operating room such as AMIGO (50). Another benefit of surgical robots and virtual workstations is that, with the importation of patient-specific imaging and other data, they permit surgical planning and, in their simulation mode, risk-free rehearsals of complex neurosurgical procedures.
The most rapidly expanding aspect of stereotactic neurosurgery in the last few years has been incorporating robots into the neurosurgical procedure, both cranial and spinal (10; 33). The cranial indications are primarily brain biopsies and deep brain stimulation electrode placement. The spinal indication is primarily minimally invasive spinal instrumentation (49). An ongoing (as of 2024) multicenter prospective study in Europe (European Robotic Spinal Instrumentation - EUROSPIN) should provide more data on the potential benefits of robotic spinal instrumentation (48). The accuracy of robotic stereotactic neurosurgery (eg, in comparison with frame-based techniques) has been confirmed (33; 47).
Advances in intraoperative imaging and laser and ultrasound technologies are increasing the scope of stereotactic neurosurgery. Laser interstitial thermal therapy (using a stereotactically placed laser fiber into the target) combined with MR thermography allows precise thermal ablation for indications ranging from movement disorders to tumor ablation (16; 20; 40). Magnetic resonance-guided laser interstitial thermal therapy may offer an alternative to stereotactic radiosurgery for some indications. Magnetic resonance-guided focused ultrasound offers the potential for not only minimally invasive ablation of deep-seated tissue (24) but also the possibility of focal opening of the blood-brain barrier to enhance the delivery of chemotherapeutic agents and other drugs (32). A comprehensive review of magnetic resonance-guided focused ultrasound has been published (26), although the technology is constantly advancing (04).
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.
Russell J Andrews MD
Dr. Andrews of the NASA Ames Research Center has no relevant financial relationships to disclose.
See Profile
Matthew Lorincz MD PhD
Dr. Lorincz of the University of Michigan has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
General Neurology
Jan. 23, 2025
General Neurology
Jan. 13, 2025
General Neurology
Jan. 13, 2025
General Neurology
Jan. 13, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 08, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 07, 2025
General Neurology
Dec. 30, 2024
General Neurology
Dec. 28, 2024