General Neurology
Use of focused ultrasound in neurologic disorders
Jan. 13, 2025
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
The author reviews the various manifestations and causes of vertical gaze palsy. These can affect upgaze, downgaze, or both, usually affecting saccades primarily. The localization can be at the brainstem, cranial nerve, neuromuscular junction, and extraocular muscles. When acquired, they imply lesions of supranuclear vertical gaze structures in the rostral midbrain and can be associated with other signs of the pretectal (Parinaud) syndrome. Degenerative disorders like progressive supranuclear palsy and metabolic disorders like Niemann-Pick type C are other causes of vertical gaze palsy.
• Vertical gaze palsies are due to damage to pre-motor structures in the midbrain, namely the rostral interstitial nucleus of the medial longitudinal fasciculus and the interstitial nuclear of Cajal. | |
• Vertical gaze palsies can involve upgaze, downgaze, or both. | |
• Parkinsonism with vertical gaze palsies is most often due to tauopathies, such as progressive supranuclear palsy and corticobasal degeneration. | |
• Several genetic defects can cause cerebellar ataxia with vertical gaze palsies, such as Niemann Pick type C disease. |
The term “gaze palsy” is best restricted to deficits in conjugate eye movements that affect both eyes. Thus, strictly unilateral problems, such as palsies of cranial nerves III, IV, or VI, are not gaze palsies, even though they do affect gaze. Likewise, impairments in vergence control, such as convergence or divergence insufficiency, are not gaze palsies, as they do not involve conjugate eye movements.
A fundamental distinction is between vertical and horizontal gaze palsies. Most gaze palsies affect one direction in one plane of eye movement only, reflecting the separation of the prenuclear control systems for vertical and horizontal eye movement. Reduction of eye movements in all planes is best termed “generalized ophthalmoparesis” and typically has an etiology distinct from those causing gaze palsies. These reductions are most commonly myopathic, occurring with mitochondrial disorders (chronic progressive external ophthalmoplegia, Kearns-Sayre syndrome, MELAS), muscular dystrophies (myotonic dystrophy, oculopharyngeal dystrophy, congenital fibrosis), myasthenia gravis, or thyroid eye disease, among others.
The term “gaze palsy” requires further elaboration. There are many different types of conjugate eye movements, including saccades, pursuit, optokinetic, and vestibulo-ocular responses. The anatomic systems that control these diverge and converge at various levels, and it is possible for some lesions to impair some eye movement systems and spare others. Hence, a left saccadic palsy is a selective gaze palsy affecting only leftward saccades but not leftward pursuit or vestibulo-ocular response. A palsy affecting all types of eye movements should be designated as a nonselective gaze palsy. Most vertical gaze palsies are selective in nature.
In contrast, the terms “partial” or “complete” when applied to gaze palsy indicate whether some motion across the midline in the paretic direction is present.
Vertical palsies usually appear selective, affecting primarily saccades. However, though clinical testing often shows sparing of pursuit and vestibulo-ocular range, quantitative testing of eye movements shows that this selectivity is relative and not absolute (87). Pursuit gain and vestibulo-ocular reflexes are impaired in many patients, though dissociable. Upgaze palsy is most frequent, combined upgaze and downgaze palsy is next in frequency, and pure downgaze palsy the most unusual (23).
Associated signs include those localizing to the rostral midbrain where the vertical gaze centers are located. These include pupillary or ocular motor signs of partial nuclear or fascicular third palsies (27; 17), including rarely a wall-eyed bilateral internuclear ophthalmoplegia (88), impaired convergence, and skew deviation (80; 92). Somnolence or even a transient fluctuating coma at onset reflects damage to the reticular activating system (27; 23; 17). Behavioral disturbances from thalamic damage include hemineglect, amnestic syndromes (23; 17), akinetic mutism, or subcortical demented states with apathy and slowness of thought (48).
Selective downgaze palsy can be associated with convergence, accommodative responses, and the pupillary near response impairment (32). The pupillary light response can be affected (32) or preserved (76). Skew deviation and internuclear ophthalmoplegia can occur (32).
In combined up and downgaze palsy, vertical vestibulo-ocular response frequently appears normal (26; 69; 76; 105; 21), but it is sometimes absent (17) or impaired in one direction alone (48). Torsional and vertical nystagmus may occur if the interstitial nucleus of Cajal is involved (80). Bell phenomenon can be absent (69) or inverted (80).
The pretectal syndrome, also called dorsal midbrain syndrome, combines vertical supranuclear palsy, affecting either upgaze alone or both upgaze and downgaze, sparing vestibulo-ocular response range, with a variable number of other signs (52). These include light-near pupillary dissociation, with loss of the pupillary light reactions from damage to the pretectum, Collier lid retraction sign, and skew deviation. Horizontal conjugate eye movements are spared, but there may be esotropia, exotropia, or convergence insufficiency. An unusual convergence-retraction nystagmus is pathognomonic. Fragmentary pretectal syndrome, with only some of the above features, is common.
Selective or nonselective vertical gaze palsy is commonly seen in Moebius syndrome, which is characterized by bilateral facial weakness and ocular abduction deficits (83). Rarely, a patient may have a vertical impairment that spares only a single direction in one eye (ie, vertical one-and-a-half syndrome) or vertical ocular motor apraxia.
Prognosis varies with cause. With thalamic hemorrhages, there is usually some resolution over several weeks.
A 69-year-old orthopedic surgeon suffered a stroke 6 months prior to evaluation. He presented with somnolence, imbalance, and diplopia. His initial examination notes documented a right third nerve palsy and ataxic gait. His symptoms had improved but persisted. The drowsiness responded to methylphenidate.
He had no anisocoria in bright light or darkness, and light reactions were intact. He had no ptosis but developed lid retraction in attempted upgaze (Collier sign). Neither eye elevated more than 10% past midline, whether saccades, pursuit, oculocephalic reflex, or Bell phenomenon were tried. Downgaze was also absent except for Doll eye maneuver, indicating that downward vestibulo-ocular response was relatively spared. The right eye had only 50% of normal adduction range, which was not improved by convergence. Horizontal saccades and pursuit were otherwise normal. He was intermittently drowsy during examination, and his gait showed a wide-based ataxia requiring support.
His ocular signs represented a combination of right third nuclear palsy, with impaired adduction and bilateral elevation paresis, and a supranuclear downgaze palsy. The sparing of downward vestibulo-ocular response confirmed that this was a supranuclear defect, most likely due to involvement of the riMLF. Conversely, the lack of upward vestibulo-ocular response suggested that upgaze palsy is not due only to riMLF or interstitial nucleus of Cajal involvement but likely the third nucleus itself. Third nuclear lesions affected both the ipsilateral superior rectus subnucleus (which innervates the contralateral eye) and decussating fibers from the contralateral superior rectus subnucleus.
His MRI showed bilateral lesions of the thalamomesencephalic junction, consistent with a “top of the basilar” stroke affecting both paramedian thalamic arteries.
The rostral mesencephalon has medial structures that provide vertical gaze inputs to the ocular motor nuclei (76; 80; 18).
The riMLF has excitatory burst neurons for vertical saccades. It receives control inputs from long-lead burst and omnipause neurons in the paramedian pontine reticular formation. The neurons for upward saccades are lateral to those for downgaze (26; 76; 80). This may explain why upgaze is sometimes spared with bilateral riMLF lesions. An alternative explanation is that upgaze motor neurons receive bilateral input from these prenuclear structures, whereas downgaze ones do not and, hence, are more vulnerable to partial destruction of the riMLFs (18).
The interstitial nucleus of Cajal performs several functions. It mediates vertical smooth pursuit with inputs from lower brainstem and cerebellar structures that traverse the brachium conjunctivum and the medial longitudinal fasciculus. It also takes vertical and torsional velocity commands to determine the firing rates to hold gaze steady in eccentric vertical positions.
Although the interstitial nucleus of Cajal forms part of an indirect vertical vestibulo-ocular response pathway, the pathway projects from the vestibular nuclei directly to the third and fourth nuclei through the medial longitudinal fasciculus and the brachium conjunctivum. The projections to ocular motor nuclei from the riMLF and interstitial nucleus of Cajal for upward movements decussate in the posterior commissure, but not those for downgaze.
Upgaze palsy. This is frequent with unilateral lesions at either the thalamomesencephalic junction (20; 23), or the posterior commissure, or its nucleus (26). There are often other signs of the pretectal syndrome. A lesion of the periaqueductal grey matter rarely causes this, perhaps by destroying descending outputs from the riMLF (94). Rarely, it occurs as a transient effect of right frontoparietal lesions, with bilateral ptosis (10).
Downgaze palsy. This occurs with bilateral dorsomedial lesions of the rostral interstitial nucleus of the medial longitudinal fasciculus (26; 23). It is hypothesized that bilateral lesions extending laterally impair upgaze also; therefore, selective downgaze palsy must require a small and specific lesion, accounting for its rarity (76).
Combined up and down gaze palsy. The lesions involve the riMLF or the interstitial nucleus of Cajal, most frequently bilaterally. In the less common unilateral cases the lesion of the ipsilateral riMLF likely also interrupts decussating fibers from the contralateral riMLF.
Vertical one-and-a-half and other syndromes. Rarely a patient may have a vertical impairment that spares only a single direction in one eye. Supranuclear bilateral downgaze paresis affecting all movements combined with monocular elevator palsy occurs with bilateral midbrain infarction (36). The opposite, supranuclear bilateral upgaze paresis with monocular depressor palsy, has also been described with unilateral midbrain infarctions (22; 60; 49). A unique case of ipsilateral monocular elevator paresis and contralateral monocular depressor paresis, combined with mild bilateral ptosis, has been reported (101). Finally, a patient with supranuclear vertical palsy combined with complete ophthalmoplegia of one eye has been described, with the ophthalmoplegia attributed to a combination of oculomotor nerve palsy and pseudoabducens palsy (95).
Vertical congenital ocular motor apraxia (82; 25) has been related to perinatal hypoxia (51) or bilateral mesencephalic-diencephalic lesions (39). Combined vertical and horizontal ocular motor apraxia can be seen in conditions such as Joubert syndrome (96).
Neurovascular disease. Infarction in the territory of the paramedian artery (a “top of the basilar” syndrome) can cause any vertical gaze palsy. This can occur with unilateral lesions (05). Brainstem ischemia is the likely mechanism of slowed saccades or reduced gaze range in vertical or all directions following cardiac surgery, though MRI and CT imaging are usually unremarkable (90). Diffusion-weighted imaging can be particularly helpful with this discrete lesion (86). Thalamic hemorrhage, especially with intraventricular extension, is a common cause (92). Associated signs of fixed pupils, horizontal gaze problems, and skew deviation are more common with hemorrhages than infarcts.
The most common cause is progressive supranuclear palsy.
In this condition, gaze palsy and early postural instability may be a marker of a variant with shorter lifespan and different tau isoforms (102). Demonstration of slowing of both vertical and horizontal saccades on eye movement recordings may be useful in differentiating this condition from Parkinson disease (77). Comparisons of the pathology of parkinsonian syndromes show greater midbrain atrophy when there are vertical gaze abnormalities to point to progressive supranuclear palsy (91). A functional MRI study demonstrated decreased glucose metabolism in the anterior cingulate gyrus in progressive supranuclear palsy patients with downgaze palsy (07). There is accumulating evidence that progressive supranuclear palsy is a disorder involving the tau protein primarily (37); interestingly, vertical gaze palsy has also been reported in other “tauopathies,” such as corticobasal degeneration (54); indeed, up to half of patients with corticobasal degeneration have vertical gaze palsies early in their course (59).
Other rarer degenerative conditions with vertical gaze palsy include parkinsonism-dementia complex (68), sometimes of the frontotemporal variety (89), dentatorubral pallidoluysian atrophy (40), and rarely dementia with Lewy bodies (63; 31). Mild vertical gaze palsy is seen in about a quarter of patients with multiple system atrophy (08). A variant of amyotrophic lateral sclerosis causes slowed vertical saccades (09; 55) and vertical gaze palsy (97). Two cases of vertical supranuclear gaze palsy during deep brain stimulation following incorrect electrode positioning were described by Fleury and colleagues (42).
Infection. Infectious or para-infectious conditions include paraneoplastic encephalitis (15), prion disease (65; 56), Whipple disease (79), and HIV encephalitis (53). Vertical gaze palsy can also occur uncommonly in sporadic or familial variants of Creutzfeldt-Jakob disease (78).
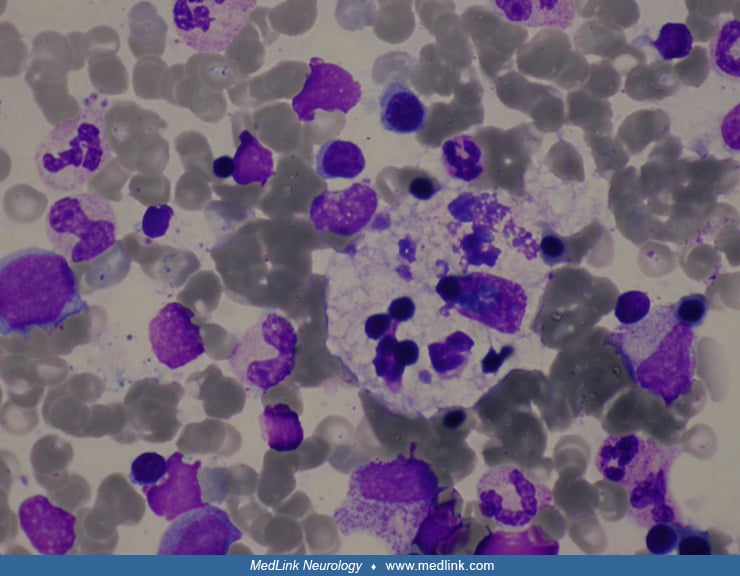
Genetic. Genetic defects with vertical gaze palsy include several conditions that share a predominance of cerebellar features. Chief among these is Niemann-Pick type C (33).
This usually presents in childhood (average age at diagnosis is 10 years) and is preceded by jaundice and hepatosplenomegaly at birth in about half of patients; vertical gaze palsy is present in 70% to 80% of patients (43; 72). However, the issue may be one of detection because eye movement recordings in five children with Niemann-Pick type C demonstrated abnormal vertical saccades in all of them, including in three without clinical abnormalities on neurologic examination (19). Juvenile and adult-onset cases have been reported to constitute 25% of cases (62). In older-onset cases, visceral signs are less common; these cases present with initial psychiatric or cognitive problems, dyslexia, cerebellar ataxia and dysarthria, dysphagia, and, less commonly, seizures and dystonia (99). In one series of Niemann-Pick type C diagnosed in adults, 94% had vertical gaze palsy on clinical examination at time of diagnosis, though most patients did not have symptoms referable to this, nor had they noticed it (62). In a cohort of patients with young adult–onset degenerative ataxia, cognitive decline, and vertical gaze palsy, four of 13 (31%) had Niemann-Pick type C (85). Dementia and death in mid-adulthood are common, but the natural history is highly variable across subjects. In 90% of patients, this is due to a mutation in the NPC1 gene, the remainder are due to NPC2 mutations. The NPC proteins are involved in intracellular trafficking of cholesterol systemically and sphingolipids in the brain (99). Another rare autosomal recessive condition consists of cerebellar ataxia and dysarthria, myoclonus and seizures, and sensory neuropathy and upgaze palsy (93). A hereditary degenerative disorder has been described in Newfoundland, with manifestations in childhood or early adulthood of impaired downgaze followed by lower limb spasticity and then ataxia, dysarthria, and dysphagia (46).
Other genetic conditions fall under the rubric of early-onset parkinsonism. Kufor Rakeb disease is an autosomal recessive condition with levodopa-responsive parkinsonism, pyramidal signs, dementia, and upgaze palsy, with onset in the teens and often death in early adulthood; it has been reported in Jordan (103) and Chile and has been associated with mutations of the ATP13A2 gene at the PARK9 locus (13). The vertical gaze palsy is useful in distinguishing this entity from several other early-onset autosomal recessive parkinsonian syndromes (70). Perry syndrome is a rare autosomal dominant Parkinsonism with respiratory failure due to a mutation in the DCTN1 gene, and in some can be associated with a downgaze palsy (64). Pantothenate kinase-associated neurodegeneration, a slowly progressive disease beginning in childhood and characterized by dystonia, parkinsonism, spasticity, retardation, and visual loss, can also cause impaired vertical saccades and pursuit (24).
Other. Rare causes include encephalitis, brain abscess, trauma, transtentorial herniation, and Wernicke encephalopathy (52). There is one case of pachymeningitis associated with rheumatoid arthritis mimicking progressive supranuclear palsy (03). Iatrogenic vertical gaze palsy has been described after implantation of depth electrodes for stimulation, presumably due to damage to the riMLF (01).
• Myasthenia gravis is one of the most common causes of ophthalmoplegia. | |
• Botulism can also cause conjugate gaze limitations mimicking gaze palsies. | |
• Thyroid eye disease can first present as upgaze palsy. |
Generalized ophthalmoparesis overlaps clinically with combined vertical and horizontal gaze palsy but is usually due to muscle or neuro-muscular junction disease. Mitochondrial disorders (chronic progressive external ophthalmoplegia, Kearns-Sayre syndrome, MELAS) and muscular dystrophies (myotonic dystrophy, oculopharyngeal dystrophy, congenital fibrosis) are rare causes of this.
Myasthenia gravis can also mimic gaze palsy, though this is usually an asymmetric disease with complaints of diplopia. Variability and fatigability are key aspects that point to a neuromuscular junction problem. Ptosis develops eventually in most patients with myasthenia. Proximal limb or bulbar weakness with fatigability are helpful but will not be present in ocular myasthenia. Single-fiber electromyography, repetitive nerve conduction studies, and assays for antibodies to acetylcholine receptor are useful tests, but the sensitivity of each of these is only 70% or less when myasthenia is confined to the eye muscles (100; 41; 61). The American Academy of Neurology published a practice advisory in 2020 on the role of thymectomy in patients with myasthenia gravis (47). Thymectomy should be discussed with patients with positive acetylcholine antibodies generalized myasthenia gravis, and minimally invasive techniques should be considered (level B). A small study showed that certain thymus pathologies may help in predicting the progression to generalized myasthenia gravis after thymectomy (108).
Botulism is another neuromuscular junction problem that affects the ocular motor system. Signs of cholinergic autonomic hypofunction such as dilated unreactive pupils, urinary retention, and decreased bowel sounds are important clues.
Miller-Fisher syndrome is a triad of ophthalmoplegia, ataxia, and areflexia, sometimes following an upper respiratory or gastrointestinal tract infection by a few weeks (16). A symmetric paresis of upgaze is a common early presentation, though with time other eye movements are usually affected too (04). Sometimes the ocular motor defects occur without ataxia, and rare cases of vertical gaze palsy in this situation have been described (57). Anti-GQ1b antibodies are present in serum (30; 29; 104).
Graves ophthalmopathy often causes restriction of the inferior recti, occasionally mimicking an upgaze palsy. Furthermore, the lid retraction in Graves can be confused with Collier sign. A key difference is that the lid retraction in Graves often increases in downgaze (lid lag) rather than in upgaze. Proptosis and conjunctival injection are other helpful clues pointing to thyroid disease (12). Most patients are hyperthyroid, but some are hypothyroid, and 15% are even euthyroid (106). Seventy-five percent already have a history of thyroid dysfunction (45), but this can follow ophthalmopathy months later. One of the major breakthroughs in the treatment for thyroid eye disease was the FDA approval of Teprotumumab (38). This randomized, double-masked, placebo-controlled, phase 3 multicenter trial concluded that among patients with active thyroid disease, teprotumumab improved proptosis, double vision, and quality-of-life when compared to placebo. There were no serious adverse events observed. However, there have been case reports of otologic symptoms, such as hearing loss (06; 14).
Imaging of the midbrain and the thalamomesencephalic junction is key to the diagnosis of vertical gaze palsies. MRI is preferred and will detect most cases with vascular or neoplastic origin. Gaze palsy in parkinsonian conditions like progressive supranuclear palsy correlate with midbrain atrophy, creating the “morning glory sign” (02).
In cases with gradual or subacute onset, disorders of muscle, neuromuscular junction, or peripheral nerves should be considered. Their tests are listed in the section on differential diagnosis.
Progressive supranuclear palsy is a neuropathologically defined disease requiring tau inclusions in glia and neurons and other specific pathological features for definitive diagnosis. Thus, premorbid diagnoses made on clinical grounds are at best “possible progressive supranuclear palsy” (50). The phenotypes are broad, with some sparing eye movements or having late-onset ocular motor abnormalities (81). However, Richardson syndrome, with its characteristic supranuclear vertical gaze palsy, is the phenotype of most autopsy-proven cases (58). MRI features have been proposed, but these are based on small studies and have not been validated against pathological diagnoses (11). Reduced midbrain volume is significantly associated with greater ocular motor dysfunction in patients with progressive supranuclear palsy (75).
If Niemann-Pick type C is suspected based on cognitive and cerebellar dysfunction associated with vertical gaze palsy consensus, clinical management guidelines recommend screening suspected cases with plasma biomarkers and confirming the diagnosis genetically (44). Widespread signs of motor neuron dysfunction are usually present in the patients with amyotrophic lateral sclerosis and can be confirmed with electromyography.
After treatable causes have been investigated and managed, symptomatic treatment of vertical gaze limitations can be considered. Progressive lenses or bifocals are of limited utility in patients who cannot move their eyes to use the appropriate part of the lens. They may find single-vision glasses for different tasks to be more effective. Some patients with limited downgaze complain of trouble reading. This can be helped with base-down prisms in both lenses of their reading glasses. Another strategy is to use a music stand or other device to place the reading material in primary gaze. Upgaze limitation rarely requires symptomatic treatment. Unilateral prisms can help eliminate diplopia in those with asymmetric ocular alignment if there is an associated skew deviation or third nerve palsy.
Studies have shown that Miglustat (Zavesca®) therapy was associated with a stabilization of neurologic manifestations in most patients with Niemann-Pick disease type C (71). Eye movement recordings have been used as a component of the monitoring of efficacy of treatment (73; 84). Animal models studies have shown that HPβCD appears to reduce cholesterol and lipid accumulation in the CNS and prolongs survival times in Niemann-Pick disease type C (74; 98). A phase 1/2 trial with intrathecal administration of HP-beta-CD has been completed (67).
Ophthalmic lubricants and sunglasses are useful to treat dry eyes and photosensitivity, respectively, in progressive supranuclear palsy. A gamma aminobutyric acid (GABA) agonist including zolpidem, eszopiclone, was reported to mildly improve ocular motor deficits and saccadic speed in progressive supranuclear palsy, but this has not been confirmed in other studies (34; 28). Some physiotherapists have suggested that eye movement exercises can improve gaze control in progressive supranuclear palsy (107), although this is not widely accepted. There is no effective disease-modifying therapy for progressive supranuclear palsy though many approaches are under active investigation (66). Drug development for progressive supranuclear palsy disease-modulating trials has focused on inhibiting posttranslational modifications of tau, enhancing immune-mediated clearing, stabilizing microtubules, or reducing levels of expression through gene therapies (35).
These are dependent on the underlying etiology.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.
Yin Allison Liu MD PhD
Dr. Liu of University of California, Davis has no relevant financial relationships to disclose.
See Profile
Heather E Moss MD PhD
Dr. Moss of Stanford University has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
General Neurology
Jan. 13, 2025
General Neurology
Jan. 13, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 08, 2025
Neuro-Ophthalmology & Neuro-Otology
Jan. 07, 2025
General Neurology
Dec. 30, 2024
Neuro-Oncology
Dec. 13, 2024
General Neurology
Dec. 13, 2024
General Neurology
Dec. 13, 2024